-
Is everyone who works behind the pharmacy counter a pharmacist?
No. Pharmacy staff can include pharmacy technicians and/or pharmacy assistants. Pharmacy technicians support pharmacists with daily technical functions so that pharmacists can use their medication expertise to focus on patient care. Pharmacy technicians perform duties that do not require clinical judgement such as counting pills, preparing drugs, entering drug orders, controlling pharmacy inventory, checking other technicians’ work, maintaining the function of complex equipment and obtaining insurance authorizations. Pharmacy technicians are licensed pharmacy professionals who are regulated by the College. They can be employed in every practice setting where there is a pharmacy including community, hospital and long-term care pharmacies.
Pharmacy assistants help in the pharmacy by supporting the work of pharmacists and pharmacy technicians, under the supervision of a pharmacist. Pharmacy assistants are not licensed or regulated by the College.
-
Why is the College implementing the new Practice Review Program?
The College is implementing the Practice Review Program in order to enhance the quality of pharmacy practice by improving compliance through strengthened enforcement. One of the ways that the College can ensure best practices are being followed is to establish and communicate standards and guidelines to pharmacy professionals and review their individual performance in a pharmacy setting. By reviewing real practice in real time, the College is helping to maintain and elevate public confidence in the profession.
-
Who has been involved with the development of the Practice Review Program?
The Board has consulted widely on the program, and was actively informed not only by the Quality Assurance Committee, but by the 1500 practising pharmacy professionals across the province who participated in an online engagement opportunity. Pharmacy managers and pharmacy professionals in community pharmacy practice also participated in two feedback forums held in April 2014.
At the April 2014 meeting, the Board established the Practice Review Committee which will oversee the development of the program, and its policies and processes for final approval by the Board.
-
How will the Practice Review Program work?
The Practice Review Program will have two components: the Pharmacy Review and the Pharmacy Professionals Review. The Pharmacy Review component will be a familiar process, as it mirrors the College’s current pharmacy inspection process. For the Pharmacy Professionals Review, a College compliance officer will observe and assess individual pharmacy professionals in four key areas of practice. Compliance officers will ensure that pharmacies meet College standards/guidelines and that pharmacy professionals are appropriately applying their knowledge, skills, and abilities to deliver consistent pharmacy care.
With the new program, pharmacy managers and pharmacy professionals will receive advance notice of a Practice Review and will know what will be reviewed. Pharmacy managers and professionals will also receive their results once the review is completed.
-
What if there are scheduling conflicts for staff who are sick or on holidays?
The College understands that at certain times of the month or year it may be inconvenient to have compliance officers in pharmacies for an extended period of time. The College will do its best to work with the pharmacy manager to determine the least disruptive times, but it is the pharmacy manager’s responsibility to ensure that most, if not all, staff are present during the Practice Review.
In the event where pharmacy professionals miss the Practice Review, a compliance officer will return to the pharmacy to perform those reviews.
-
What is the College looking for during the Pharmacy Review?
Compliance officers will be reviewing pharmacies for adherence to practice standards and guidelines such as the Health Professions Act, College Bylaws, the Model Standards of Practice, the Pharmacy Operations and Drug Scheduling Act, Professional Practice Policies, and the Framework of Professional Practice and guidelines
-
What is the College looking for during the Pharmacy Professionals Review?
Pharmacy professionals will be reviewed on focus areas that have been deemed the most relevant to professional pharmacy practice in British Columbia. The Board has identified a total of six focus areas they believe to have the greatest impact on public safety. Focus areas differ between pharmacists and pharmacy technicians. Each will be reviewed on four focus areas depending on their registration type:
The focus areas for pharmacists are:
- Patient Identification Verification
- Profile Check
- Counseling
- Documentation
The focus areas for pharmacy technicians are:
- Patient Identification Verification
- Product Distribution
- Collaboration
- Documentation
-
What criteria or specific details will the College be looking for under each of these four focus areas?
For information on specific assessment criteria, please refer to the following review forms:
For Hospital Pharmacy:
- Hospital Pharmacy Review Form
- Hospital Pharmacist Review Form
- Hospital Pharmacy Technician Review Form
For Community Pharmacy:
-
What happens after the review has been completed?
After the review has been completed, the compliance officer will forward the Pharmacy Review results to the pharmacy manager, and individual Pharmacy Professional Review results to each pharmacy professional. These results will be available in real time, accessible online through the confidential and secure eServices portal. The compliance officer will discuss results with the pharmacy manager and individual pharmacy professional for their respective reviews.
Where a compliance officer observes a standard/guideline that is not met, they may assign action item(s). These observations and action items are standardized to ensure consistency and fairness of all practice reviews. Pharmacies and pharmacy professionals will be given deadlines (typically 30 days) to complete these items, and compliance officers will verify whether the action items have been completed by the deadline. After all action items have been completed, the compliance officer will sign-off on the review, and a notice of completion will be issued to the appropriate party.
-
When is the Practice Review Program being launched?
The Practice Review Program launched in Community Practice in 2015 and in Hospital Practice in 2017.
-
How will pharmacy professionals who do not practice in a conventional community or hospital setting be reviewed?
The College recognizes that there are a variety of different practices in BC, and asked for feedback on this subject through online engagement with over 1500 pharmacy professionals. The College will be taking a phased approach in developing the Practice Review Program and, with input from the Practice Review Committee, will develop processes that address different practices within the province.
-
What happens to the authorized refills when a prescription is adapted?
The pharmacist takes responsibility for the adapted prescription as well as the authorized refills. The pharmacist could choose to provide an initial adaptation of the prescription but reduce or eliminate the authorized refills. If they did this they would need to provide the rationale for their decision in their documentation and inform the patient that they will need to return to their physician earlier than intended (note: a pharmacist cannot add refills that were not initially authorized by the prescriber). Whatever the final decision is, it must be properly documented and provided in the notification to the prescriber.
If the pharmacist adapts the prescription and maintains the authorized refills, when the patient returns for a refill the pharmacist would process the refill as they would any other refill prescription. The processing of a refill of an adapted prescription is not considered an adaptation per se, so the documentation and notification requirements of PPP-58 do not apply.
Should the patient return to the pharmacy for a refill and a different pharmacist is on duty that pharmacist would again process the refill as they would any other refill, keeping it under the adapting pharmacists ID. If they have a concern about the appropriateness of the adapted prescription they should do what they normally do if they have a concern about refilling a prescription; refuse to fill, provide an emergency fill if necessary and in this case either refer the patient back to the adapting pharmacist or to the original prescriber.
Finally it is important to note that when a pharmacist adapts a prescription and maintains the authorized refills they must inform the patient that as a result of them doing this the prescription is now non-transferable which means the patient will need to return to this specific pharmacy in order to get their refills.
-
How can I safely and effectively measure small doses of methadone 10mg/ml volume?
The pharmacist must measure the methadone dose using a calibrated device with an error rate of no greater than 0.1ml, which is equal to 1mg. All devices used to measure methadone should be distinctive and recognizable and should be used only to measure methadone solutions. Devices should be labelled with a “methadone only” label and a “poison” auxiliary label with the international symbol of the skull and cross bones. Pharmacists may contact their wholesaler for assistance to locate a product that meets the required specifications.
-
Can I ask my pharmacist about correct dosing and possible side effects of common over-the-counter (non-prescription drugs), supplements and herbal remedies?
Yes. Please talk to your pharmacist. Too few patients take advantage of the pharmacist's knowledge and ask questions about non-prescription drugs and alternative therapies.
-
Why does the pharmacist ask me questions about my medical conditions? Do they really need to know that?
Your pharmacist’s main responsibility is to find, fix and prevent drug related problems. Many medications can be used for more than one medical condition. In order to ensure that your medications are appropriate for you and that you will get the most benefit from them, your pharmacist has to understand why you are taking the medications.
-
Sometimes my pharmacist phones my doctor with some questions. Why do they need to bother the doctor?
Your pharmacist’s main responsibility is to find, fix and prevent drug related problems. Many medications can be used for more than one medical condition. In order to ensure that your medications are appropriate for you and that you will get the most benefit from them, your pharmacist has to understand why you are taking the medications. Sometimes they need to contact your doctor to confirm the reason the medication has been prescribed, or they may have some suggestions on a different medication or a different dosage that might work better for you. They may also want to talk the doctor about the other medications you are on, especially if there is a possibility of an interaction between two or more of your medications.
-
Why does my morphine prescription need to be written on a duplicate/triplicate prescription form?
There are specific classes of drugs under the Controlled Prescription Program (including narcotics) which have the potential for inappropriate use. These drugs must be written on a Controlled Prescription Program form for tracking purposes to reduce the potential for inappropriate prescribing and to prevent forgeries.
-
When do I need to pre-register with the College?
Pre-registration with the College of Pharmacists of BC is required prior to registering for the Bridging Program for those on the ‘Current Technicians’ path. The application form for pre-registration is available on the College website.
-
Which post-secondary institutions are currently offering a CCAPP Accredited Pharmacy Technician Program?
Please check the CCAPP website for the list of Accredited Pharmacy Technician Programs: http://www.ccappaccredit.ca/accredited_programs/technician/history_by_program/ and the College website for more information.
-
I just received a prescription written by a nurse practitioner from Alberta. Do out-of-province nurse practitioners have prescribing privileges in B.C.?
No, out-of-province nurse practitioners are not recognized prescribers in BC. In order to prescribe, a person must be a “practitioner” as defined by PODSA. While BC nurse practitioners are authorized under the provincial Health Professions Act to prescribe, out-of-province nurse practitioners do not fall within the definition of a “practitioner” in BC.
Depending on the drug and the situation, pharmacists should use their professional judgment to decide if it is appropriate to process a new or transferred nurse practitioner (out-of-province) prescription as an emergency supply prescription using the pharmacist’s ID as the prescriber. In all cases, clearly document the situation on the prescription.
-
Can I fill a prescription using product compounded by another pharmacy?
Pharmacists who do not provide specialty compounding services have two options:
1. Refer the patient to a pharmacy that can prepare the product.
2. Obtain the specialty compound by contracting with another pharmacist who provides the service. A contract between the two pharmacies must be signed and retained by both pharmacy managers if the service is contracted out.
If you have any questions or concerns, please email [email protected].
-
I suspect my coworker may have a substance use issue. Do I need to report this to the College?
I think that a pharmacist may have a substance use issue. I've never seen him use drugs on the job but his behaviour and appearance indicate that there may be a problem. He makes a lot of dispensing errors and since I hired him, I've noticed that a number of narcotics have been missing. Do I need to report this to the College even if I'm not sure that he has a substance abuse disorder and even though I'm not sure he is the cause of the missing narcotics?
Section 32.1 to 32.4 of the Health Professions Act states that “If a practitioner or registrant has reason to suspect that a person registered under this Act is suffering from a physical or mental ailment or an excessive personal use of alcohol or drugs that might constitute a danger to the public, the practitioner or registrant must immediately report this to the registrar.” This means that even if you don’t know for sure that a problem exists, but you have reason to be suspicious, you must report your concern to the college. College staff will ask you a number of questions and may suggest strategies for improving your monitoring systems so you can find out more about what is happening to your drug supply. They will also need to gather information about the pharmacist’s behaviour. If it turns out that the pharmacist does have a substance abuse problem, the College’s key interest will be to work with the pharmacist on a recovery program. This can be done through a mutual agreement with the pharmacist; an adversarial discipline process is not usually required.
-
A patient brought in a prescription for two drugs. The patient only wants me to dispense one of these drugs and wants another pharmacy to dispense the other drug. What do I need to do?
The process you need to follow is different, depending upon which drug you dispense.
Amoxil® dispensing (non-narcotic) - you need to return the original prescription to the patient:
- Process the prescription for Amoxil®.
- On the original prescription, indicate that you have dispensed the Amoxil® and note your pharmacy name, your initials, and the date.
- Photocopy the original prescription for your records.
- On the photocopy, make a note that the original prescription was returned to the patient.
- Return the original prescription to the patient. The patient can then have the undispensed narcotic prescription dispensed at the pharmacy of his/her choice.
Tylenol with Codeine No.3® dispensing (narcotic) - you need to keep the original prescription:
- Process the prescription for Tylenol with Codeine No.3®.
- Log the prescription for Amoxil®.
- Photocopy the original prescription for your records.
- On the original prescription, indicate that you have dispensed the Tylenol with Codeine No.3® and logged the Amoxil®. Note your pharmacy name, your initials, and the date.
- You may photocopy the original prescription and provide the photocopy to the patient. Be sure to note your pharmacy name and telephone number on the photocopy so that the other pharmacy can contact you to transfer the Amoxil® prescription.
-
How does conscientious objection work in pharmacy practice?
If a pharmacy professional declines to provide a pharmacy service on the basis of a conscientious objection, he or she is required to adhere to the Colleges’ Code of Ethics, Standard 1 (g)(iii), cooperating in effective transfers of care initiated by the patient (without needing to make a referral).
Pharmacy professionals need to inform their pharmacy manager and employer of a conscientious objection either before they accept employment or at the earliest opportunity.
Pharmacies should have a process in place to ensure that in the case where a pharmacy professional conscientiously objects to providing a service, the patient can be directed to an alternate provider for the service in a timely manner.
Standard 1: Registrants Protect and Promote the Health and Well-Being of Patients
(g) Registrants must provide pharmacy services requested by patients and may only refuse to provide these services for any of the following reasons:
(iii) the provision of the product or service is contrary to the sincerely held conscientious or religious belief of a registrant, in which case the registrant must ensure that:
- they have informed and explained to the pharmacy manager and employer of their conscientious or religious belief before they accept employment;
- if the belief is formed after employment is accepted, they inform the pharmacy manager and employer at the earliest opportunity; o they do not discuss their personal beliefs or ask patients to disclose or justify their own beliefs;
- they participate in a process designed to exercise their freedom of conscience and religion in a manner that respects the patient's right to receive products and services in a timely manner and in a way that minimizes suffering and hardship to the patient;
- they fulfill their duty of care to the patient in a manner that is nonjudgmental, continuous and non-discriminatory;
- in the event of failure of the system developed to ensure the timely delivery of the product or service, and notwithstanding the registrant’s conscientious or religious beliefs, they provide patients with enough information and assistance to allow them to make informed choices for themselves;
- they cooperate in effective transfers of care initiated by the patient and are not required to make a referral; and
- they do not rely on conscientious or religious beliefs in order to discriminate against any patient on morally irrelevant grounds including those outlined in Standard 3, Guideline g of this Code.
-
Are registered pharmacy technicians and pharmacists still required to comply with legislated requirements and their professional obligations, even if they are not working as a pharmacy technician or pharmacist?
Pharmacy technicians and pharmacists registered with the College are health professionals under the Health Professions Act and must uphold legislative requirements and professional obligations at all times.
This means that regardless of job title or role, a registered pharmacy technician or pharmacist must meet requirements under the Health Professions Act, Pharmacy Operations and Drug Scheduling Act and in the College’s bylaws. As health professionals, they are held responsible to their own scope of practice and can be subject to disciplinary action for practice issues.
-
Are all pharmacies required to comply with the new technology requirements?
Bylaw Reference: PODSA Bylaws s. 23.3(1):
23.3(1) A pharmacy may maintain electronic records containing personal health information if the pharmacy has the equipment, software and systems necessary for the input, storage, use, protection and retrieval of records that are required to be kept under bylaws of the college or other legislation that regulates the practice of pharmacy.
In addition, the detailed technology requirements are set out in s. 23.3 of the PODSA Bylaws.
A pharmacy must comply with the new technology requirements if it maintains electronic records containing personal health information. Since most pharmacies keep some form of electronic records containing personal health information, most pharmacies will be required to comply with the new technology requirements. However, pharmacies will have until May 13, 2019 to comply.
-
Are all pharmacies now required to keep electronic records?
No, pharmacies may either keep only electronic records, only hard copy records, or a combination of both. Pharmacies that keep any form of electronic records containing personal health information must comply with the new technology requirements in s. 23.3 of the PODSA Bylaws by May 13, 2019.
-
Are electronic equivalents acceptable for all College-required documentation, including invoices and documentation in respect of the purchase, receipt or transfer of drugs, confidentiality forms, narcotic reconciliation records etc.?
Yes, pharmacies may keep all records required by the College in electronic format. Only records containing personal health information are required to be maintained in a system that complies with s. 23.3 of the PODSA Bylaws.
-
Are all electronic records required to be maintained in a system that complies with the new technology requirements?
Bylaw reference: PODSA Bylaws, s.23.3(1):
23.3. (1) A pharmacy may maintain electronic records containing personal health information if the pharmacy has the equipment, software and systems necessary for the input, storage, use, protection and retrieval of records that are required to be kept under bylaws of the college or other legislation that regulates the practice of pharmacy.
Only records containing personal health information are required to be maintained in a system that complies with s. 23.3 of the PODSA Bylaws. This means that records such as invoices and documentation in respect of the purchase, receipt or transfer of drugs, confidentiality forms, narcotic reconciliation records, and other non-patient related records may be kept in electronic form in a system of the pharmacy’s choice.
-
Can electronic records be stored on a cloud? If yes, does the cloud need to be located in Canada?
The College does not have restrictions on cloud storage. However, as with all records, pharmacies must ensure that data is stored and accessed in accordance with applicable privacy law.
Pharmacies that are private-sector organizations are governed by B.C.’s Personal Information Protection Act (PIPA). PIPA does not contain restrictions on the storage of, or access to, personal information from outside Canada. Organizations subject to PIPA may therefore use cloud-based storage services outside Canada. Many community pharmacies will fall under this category.
Pharmacies that are “public bodies” are governed under B.C.’s Freedom of Information and Protection of Privacy Act (FIPPA). Public bodies covered by FIPPA are, with some exceptions, required to ensure that personal information is stored and access only in Canada. There is no exemption for cloud storage. Hospital pharmacies and pharmacies run by a provincial health authority may fall under this category. A private sector pharmacy that is under contract to a public body to provide pharmacy services for the public body may also fall under this category.
The PharmaNet database is subject to FIPPA. Therefore, any information in PharmaNet or obtained from PharmaNet must be accessed, disclosed and stored in Canada.
-
I just received a prescription written by a pharmacist from Alberta. Do out-of-province pharmacists have prescribing privileges in B.C.?
No, out-of-province pharmacists are not recognized prescribers in BC. Although some pharmacists may have certain prescribing privileges in their own provinces, a valid prescription in BC must be written by a “practitioner” as defined by PODSA. Out-of-province pharmacists do not fall within this definition of a “practitioner” in BC.
Depending on the drug and the situation, pharmacists should use their professional judgment to decide if it is appropriate to process a new or transferred pharmacist prescription as an emergency supply prescription using the pharmacist’s ID as the prescriber. In all cases, clearly document the situation on the prescription.
-
What information should be included on the business licence of the pharmacy?
The business licence must be current and valid, and must list the name of the Direct Owner, the pharmacy (operating) name, and the correct pharmacy address. If the pharmacy licence does not contain separate areas for the pharmacy name and the Direct Owner name, the following format should be used: “[Direct Owner Name] DBA [Pharmacy Name]”.
For further information on business licence requirements, refer to the Pharmacy Licensure Guide.
-
Who is responsible for uploading the business licence for a pharmacy renewal application, and how do I upload one?
The business licence can be uploaded to the Pharmacy Portal 75 days prior to the licence expiry by the Authorized Representative(s) OR the pharmacy manager. To access the pharmacy portal, log into eServices, go to ‘My Pharmacies’ and scroll to the bottom of the page. At this point, you may have one of two views depending on your role(s):
- Authorized Representative: Click the ‘+’ sign next to the name of the Direct Owner to expand the list of pharmacies owned by that Direct Owner. Find the pharmacy due for renewal and click on the hyperlinked pharmacy name to access the pharmacy portal. Once you are in the Pharmacy Portal, review the pharmacy information on each tab and click the ‘Next’ button to advance to the ‘Business Licence’ tab where you can upload the business licence. Once you have uploaded the document, the file name and upload date will be updated.
- Pharmacy Manager: Click on the pharmacy’s name to access the Pharmacy Portal. Once you are in the Pharmacy Portal, review the pharmacy information on each tab and click the ‘Next’ button to advance to the ‘Business Licence’ tab where you can upload the business licence. Once you have uploaded the document, the file name and upload date will be updated.
For further instruction on uploading a business licence, refer to the Pharmacy Licensure Guide.
-
My municipality does not issue a business licence. How do I complete this requirement for renewal?
If your pharmacy or telepharmacy is located in a jurisdiction that does not issue a business licence, you should provide a letter or correspondence from the jurisdiction which confirms that they do not issue a business licence. You should upload the document in place of the business licence on eServices.
For further information on the business licence requirements, refer to the Pharmacy Licensure Guide.
-
When can I submit my pharmacy renewal application?
You may submit the pharmacy licence renewal requirements once you receive your pharmacy renewal notice approximately 75 days before the pharmacy licence expiry date. You will not have access to submit the renewal requirements prior to receiving the renewal notice. You may prepare for renewal in advance by compiling any ownership documents required and ensuring your business licence meets all requirements.
For further information on what is required for pharmacy renewal, refer to the College website or the Pharmacy Licensure Guide .
-
What are the requirements for renewal?
The pharmacy licence renewal requirements vary depending on the type of ownership of your pharmacy. Most pharmacies in B.C. are owned by corporations and are required to submit the following:
- Ownership documents
- A copy of the current business licence issued by the municipality (if applicable)
- Proof of Eligibility from each Indirect Owner and the pharmacy manager
- Payment of the renewal fee
This checklist will provide details regarding the above requirements.
If your pharmacy is not owned by a corporation (i.e. hospital, university, sole proprietor, etc.), the renewal requirements will differ slightly.
For further information on renewal requirements, refer to the College website or the Pharmacy Licensure Guide.
-
How can I track the status of my pharmacy licence renewal application? Is there a way for me to see which of my Indirect Owners has not submitted a requirement?
The status of the pharmacy licence renewal application can be tracked on eServices by either the Authorized Representative(s) or the pharmacy manager. Indirect Owners of the pharmacy will not be able to track the renewal status, or see the status of their Proof of Eligibility. Indirect Owners should reach out to their Authorized Representative(s) if they have questions about the renewal status of a pharmacy. The steps taken to access this information on eServices by the Authorized Representative(s) or pharmacy manager are different depending on your role(s). However, note that only the Authorized Representative(s) of the pharmacy can see who has and has not submitted their attestation and/or Criminal Record History (CRH).
- Authorized Representative: Log into eServices and go to ‘My Pharmacies’. Scroll down and expand the list of pharmacies by clicking on the ‘+’ sign next to the name of the Direct Owner. Once you have expanded the list of pharmacies owned by that Direct Owner, scroll down the list to find the pharmacy due for renewal. Next to the pharmacy name, you will see the status of the attestation, CRH, business licence, and payment. The status of the ownership information will be listed next to the name of the Direct Owner. To view the detailed list of Indirect Owners, click on the ‘Pending’ link under the Renewal Complete column. This detailed list will display all of the Indirect Owners and whether or not they have submitted their attestation and/or CRH. This list does not disclose the eligibility status of the attestation and CRH.
- Pharmacy Manager: Log into eServices and go to ‘My Pharmacies’. Scroll down to the pharmacy summary at the bottom of the page. This summary will provide the status of the ownership information, attestation, CRH, business licence, and payment. Note that only the Authorized Representative(s) of a pharmacy are able see a detailed view of which Indirect Owners have submitted their attestation or Criminal Record History (CRH).
Note: the ‘Attestation Summary’ and ‘CRH Summary’ statuses refers to the status of all attestations and Criminal Record History results required for the pharmacy renewal application. If one or more individuals has not submitted their attestation and/or CRH, the ‘Attestation Summary’ and/or ‘CRH Summary’ column status will show as ‘Pending’, regardless of whether you have personally submitted this information.
For further explanation of each renewal status, refer to the Pharmacy Licensure Guide.
-
Who is responsible for submitting the requirements for a pharmacy licence renewal application?
The Authorized Representative(s) is responsible for ensuring that all renewal requirements are submitted before the deadline and will have access to submit most of this information. However, all Indirect Owners (if applicable) and the pharmacy manager will have to submit Proof of Eligibility as part of the renewal application. The pharmacy manager will also have access to submit a copy of the current business licence.
The renewal status can be monitored by the Authorized Representative(s) and the pharmacy manager on their eServices account. The Indirect Owners of the pharmacy will not be able to track the renewal status, or see the status of their Proof of Eligibility. Indirect Owners should reach out to their Authorized Representative(s) if they have questions about the renewal status of a pharmacy.
For further details on tracking the renewal status can be found in the ‘How can I track the status of my pharmacy renewal application?’ FAQ.
-
What are my responsibilities as a pharmacy manager for the pharmacy licence renewal?
As the pharmacy manager, you must complete your Proof of Eligibility and you may also upload a copy of the current business licence. Proof of Eligibility consists of a yearly attestation and a Criminal Record History (CRH) which must be submitted once every 5 years. The business licence may be uploaded by either the pharmacy manager or Authorized Representative(s). As the manager, you should discuss with your Authorized Representative(s) who will be responsible for uploading the business licence on eServices before the due date.
Ensuring the submission of all other renewal requirements is the responsibility of the Authorized Representative(s) of the Direct Owner(s).
For further information about pharmacy renewal, refer to the Pharmacy Licensure Guide.
-
When is the deadline to submit the pharmacy licence renewal application?
All requirements must be received by the College no later than 30 days before the pharmacy licence expiry date. If the College has not received the requirements on or before the 30 day deadline, the pharmacy licence renewal application will be referred to the Application Committee for review and an administrative fee may be applied.
For further information on pharmacy renewal, refer to the Pharmacy Licensure Guide.
-
What happens if I do not submit all of the requirements by the renewal deadline (30 days before the pharmacy licence expires)?
Failure to submit all of the renewal requirements: ownership information, Proof of Eligibility (attestation & CRH) from the pharmacy manager and all Indirect Owners (if the Direct Owner is a corporation(s)), a valid business licence (if applicable) and payment, will result in your pharmacy licence renewal application being referred to the Application Committee for review and an administrative fee may be applied.
For further information on the Application Committee, refer to the Pharmacy Licensure Guide.
-
What is the Application Committee?
The Application Committee (AC) is a legislative committee established under the Pharmacy Operations and Drug Scheduling Act and Health Professions Act to review any pharmacy licence applications that do not meet the eligibility criteria, are incomplete, or have false or misleading information. The AC may issue, renew or reinstate a pharmacy licence (with or without conditions), or refuse to issue, renew or reinstate a pharmacy licence.
For further information on the Application Committee, refer to the Pharmacy Licensure Guide.
-
What type of applications are there? What requirements do I have to submit?
In addition to a new pharmacy licence application and renewal application, the Direct Owner needs to notify the College when the following changes to the pharmacy occur. The requirements for each type of application can be found by clicking on the application name below:
Type of Change Details Deadline to Submit Change of Direct Owner A change in ownership from one legal entity to another (including amalgamation). Minimum 30 days before the effective date of change. Change of Indirect Owner A change of directors, officers, and/or shareholders of a non-publicly traded BC corporation. Minimum 7 days before the effective date of change. Change of Manager A change in pharmacy manager. Minimum 7 days before the effective date of change. Change of Corporation Name A change in the name of the corporation, which can be either a direct or indirect owner of a pharmacy. Recommended 7 days before effective date of change. Change of Operating Name A change in the pharmacy name. Minimum 30 days before the effective date of change. Change of Location A change in the location of the pharmacy. Minimum 30 days before the effective date of change. Change in Layout A change in the layout of the pharmacy. Minimum 30 days before the effective date of change. Pharmacy Closure A permanent closure of the pharmacy. Minimum 30 days before the effective date of change. The College is considered to have received notification once a change application is received. All applications should be sent to [email protected].
For further information on the different change applications, refer to the Pharmacy Licensure Guide.
-
Who can submit a pharmacy application?
The Authorized Representative(s) of the Direct Owner of a pharmacy will be responsible for submitting licensure applications. For example, the Authorized Representative(s) of a pharmacy owned by a corporation will be the director(s) of the Direct Owner. Officers, shareholders, and pharmacy managers are not able to submit change applications.
For further information on each pharmacy application, refer to the College website or the Pharmacy Licensure Guide.
-
How do I submit a Change of Manager application? As the pharmacy manager can I submit the change request?
A Change of Manager application must be submitted through eServices by one of the Authorized Representative(s) of the pharmacy. The current pharmacy manager will not have access to make this change (unless they are also an Authorized Representative of the pharmacy). A manager change request must be submitted at least 7 days before the effective date to allow the new manager time to complete his/her Proof of Eligibility (attestation and Criminal Record History). The manager change will not be completed until the College receives the new manager’s Proof of Eligibility.
Authorized Representative(s) can follow the instructions in the Pharmacy Licensure Guide to submit a Change of Manager application on eServices.
-
My pharmacy will be undergoing multiple changes in the near future (e.g. I am changing the operating name and the layout of a pharmacy). What should I do?
If your pharmacy is undergoing multiple changes, you must submit all appropriate change applications. For example, a pharmacy that is planning to undergo renovations and is also changing the pharmacy name would submit both a Change of Layout application as well as a Change of Operating Name application. Note that applications have different notification periods and processing times which should be adhered to. For further details on application processing times, refer to the ‘What type of applications are there? What requirements do I have to submit?’ FAQ . Failure to provide enough notice to the College may result in a delay in processing or referral to the Application Committee.
For further information on submitting multiple change applications, refer to the Pharmacy Licensure Guide.
-
I am planning to make the same change (e.g. changing the Direct Owner, corporate name, etc.) for all pharmacies owned by my corporation. How should I notify the College?
If the same change applies to multiple pharmacies, you have two options to complete the change application for all applicable pharmacies:
- Submit a change application for each pharmacy affected by the same change.
- Submit a change application for one pharmacy and use Form 9: Pharmacy Licensure – Multiple Pharmacies to list all other pharmacies impacted by the same change.
For further information, refer to the Pharmacy Licensure Guide.
-
The College recently completed an inspection at my pharmacy and identified that there was a Change in Layout of the pharmacy which was not reported to the College. What process should I follow to rectify this?
Pursuant to section 4.1(3) of the Pharmacy Operations and Drug Scheduling Act, a Direct Owner must give the Registrar 30 days' written notice of any changes respecting the layout of the pharmacy.
To comply with this provision, you must complete and submit the following to the Licensure Department by email at [email protected]:
- Change in Layout application form;
- An updated pharmacy diagram;
- Pre-opening inspection report (complete up to and including the Security section only), and
- Digital evidence confirming compliance with the requirements.
All required documents and more information about the Change in Layout application process can be found on the College website, or in the Pharmacy Licensure Guide.
-
How long will it take to process my pharmacy application?
Typically the processing time for each phase of an application is 7 days. Some of the change applications have multiple phases which will add to the processing time. An application submitted without all the requirements may result in a delay in processing.
For further information on the timeline of each application, refer to the Pharmacy Licensure Guide.
-
I am relocating my pharmacy, when can I operate in the new location?
The Change of Location application must be completed before the pharmacy can operate in a new location. Pursuant to section 6(1)(b) of the Pharmacy Operations and Drug Scheduling Act, a pharmacy licence is cancelled if the location of the pharmacy changes. If the new location is open before a new licence is issued by the College, the pharmacy will be operating unlawfully.
For further information on the Change of Location process, refer to the College website or the Pharmacy Licensure Guide.
-
Where can I find the invoice for my pharmacy licence renewal application?
Only the Authorized Representative(s) have access to view invoices and submit payment for a pharmacy licence renewal. In the ‘My Pharmacies’ section of eServices, click on the name of the Direct Owner (owner of the pharmacy). Once you have submitted the ownership requirements, you will land on the payment page. This page will have a ‘Print Invoice’ option that will print a list of all pharmacies due for renewal within the chosen month.
For further information regarding printing the invoice, refer to the Pharmacy Licensure Guide.
-
Where can I find my pharmacy licence?
The pharmacy licence can be downloaded by any Authorized Representative(s) or the pharmacy manager from the Pharmacy Portal. To access the Pharmacy Portal, log into eServices, go to ‘My Pharmacies’ and scroll to the bottom of the page. At this point, you may have one of two views depending on your role(s):
- Authorized Representative: Click the '+' sign next to the name of the Direct Owner, and then the pharmacy name. On the next page you will see the 'Download Pharmacy Licence' button.
- Pharmacy Manager: Click on the pharmacy name. On the next page you will see the 'Download Pharmacy Licence' button.
For further instructions on how to download the pharmacy licence, refer to the Pharmacy Licensure Guide.
-
Do I have to report a change in pharmacy hours?
Yes, pursuant to the Pharmacy Operations and Drug Scheduling Act Bylaws, the pharmacy hours, both when a pharmacist is on and off duty, must be reported to the College. This change can be reported by either the Authorized Representative(s) or the pharmacy manager in the Pharmacy Portal. To access the Pharmacy Portal, log into eServices, go to ‘My Pharmacies’ and scroll to the bottom of the page. At this point, you may have one of two views depending on your role(s):
- Authorized Representative: Click the '+' sign next to the name of the Direct Owner, and then the pharmacy name. On the next page you must click ‘Next’ at the bottom of both the ‘Profile’ and ‘Staff’ pages to access the ‘Services’ page. You may edit the start or end time by selecting the correct time in the dropdown menu on the corresponding day of the week. To save changes, click the ‘Next’ button once all hours have been updated.
- Pharmacy Manager: Click on the pharmacy name. On the next page you must click ‘Next’ at the bottom of both the ‘Profile’ and ‘Staff’ pages to access the ‘Services’ page. You may edit the start or end time by selecting the correct time in the dropdown menu on the corresponding day of the week. To save changes, click the ‘Next’ button once all hours have been updated.
For further information on updating the pharmacy hours, refer to the College website or the Pharmacy Licensure Guide.
-
As the pharmacy manager, how do I update the pharmacy staff roster?
In order to update the roster, login to eServices, click on ‘My Pharmacies’, and then the name of the pharmacy. Once in the pharmacy portal, click the ‘Next’ button to access the staff roster. Use the ‘Add’, ‘Edit’, and ‘Delete’ buttons to update the staff roster.
Pursuant to section 18(2)(c) of the Pharmacy Operations and Drug Scheduling Act Bylaws, a manager must notify the Registrar in writing of the appointments and resignations of registrant’s as they occur by updating the pharmacy staff roster in eServices.
For further information regarding updates to the staff roster, refer to the Pharmacy Licensure Guide.
-
How do I complete my Proof of Eligibility?
Proof of Eligibility (POE) can be completed by logging into eServices, clicking 'My Profile' > 'Proof of Eligibility'. Complete the information on each of the pages, clicking ‘Next’ at the bottom of each page to navigate through the tabs. If applicable, the last tab provides instructions to complete the Criminal Record History (CRH) portion of the POE. The CRH will be completed on a third party site, and it may take up to 7 days for the College to receive the result. You will only have to complete a CRH once every 5 years. Once you have completed your POE, click the ‘Close’ button.
Note: POE must be completed on a desktop computer using one of the recommended browsers: Google Chrome or Internet Explorer.
For further information on Proof of Eligibility, refer to the Pharmacy Licensure Guide.
-
How often do I have to complete my Proof of Eligibility?
Proof of Eligibility consists of both an attestation and Criminal Record History (CRH). The attestation must be completed annually for each pharmacy, or when an individual takes on a new role within the pharmacy. The CRH must be completed once every five years.
Note that the CRH is not the same as the Criminal Record Check (CRC) that is completed by registrants of the College. All owners who are registered pharmacists as well as the pharmacy manager must also continue to undergo the separate CRC process to maintain their registration with the College.
For further information on Proof of Eligibility, refer to the College website, or the Pharmacy Licensure Guide.
-
What is a Criminal Record History (CRH) and why is it required?
CRH involves a search of criminal record history information in the databases of the Royal Canadian Mounted Police and local police stations to determine whether the eligibility criteria to hold a pharmacy licence is met. Specifically, pursuant to the Pharmacy Operations and Drug Scheduling Act (PODSA), “no direct owner, indirect owner or manager has, within the previous 6 years, been convicted of an offence under the Criminal Code (Canada)”.
If this eligibility requirement is not met by owners and managers, the pharmacy application will be referred to the Application Committee (AC) for review. After reviewing the pharmacy application, the AC may request additional information or evidence and may then issue, renew, or reinstate the pharmacy licence with or without conditions, or refuse to issue, renew, or reinstate the pharmacy licence.
The CRH search will be conducted by the Board-approved external vendor, Sterling Backcheck, a professional private criminal record check provider that partners with local police stations to provide results.
For further information on Criminal Record History, refer to the Pharmacy Licensure Guide.
-
I have completed my Criminal Record History (CRH) with Sterling Backcheck using instructions provided by the College. How do I share my results with the College? When will the College receive my results?
The CRH results will be sent directly from Sterling Backcheck to the College. Note that although you may have already received your results, it can take up to 7 days for the College to receive this information. Please do not send your results to the College; we only accept this information directly from Sterling Backcheck.
For further information on Criminal Record History results, please refer to the Pharmacy Licensure Guide. -
I have submitted my attestation and Criminal Record History (CRH). How can I check to make sure I’ve completed my Proof of Eligibility?
Only Authorized Representative(s) of the pharmacy may check who has submitted their Proof of Eligibility on eServices. Indirect Owner(s) and the pharmacy manager can either contact an Authorized Representative to confirm that their attestation and Criminal Record History (CRH) have been submitted, or they may contact the Licensure Department via email at [email protected]. Note that the Licensure Department will not disclose the eligibility status of the Indirect Owner(s) or pharmacy manager.
Authorized Representative(s) may follow the instructions below to access the Proof of Eligibility information:
- Authorized Representative: Log into eServices and go to ‘My Pharmacies’. Scroll down and expand the list of pharmacies by clicking on the ‘+’ sign next to the name of the Direct Owner. Once you have expanded the list of pharmacies owned by that Direct Owner, scroll down the list to find the pharmacy due for renewal. This initial list view will provide the status of the ownership documents, attestation, CRH, business licence, and payment. To view the detailed list of Indirect Owners, click on the ‘Pending’ link under the Renewal Complete column. This detailed list will display all of the Indirect Owners and pharmacy manager, and whether or not they have submitted their attestation and/or CRH. This list does not disclose the eligibility status of the attestation and CRH.
For further information regarding the status of your pharmacy renewal, refer to the Pharmacy Licensure Guide.
-
Who can I speak with at the College if I have questions or concerns regarding the privacy and confidentiality of my Criminal Record History (CRH) information?
The Privacy Officer at the College is responsible for ensuring compliance with the appropriate privacy legislation and can be reached at [email protected]. The College collects, uses, and discloses personal information in accordance with BC’s Health Professions Act (HPA), Pharmacy Operations and Drug Scheduling Act (PODSA), Freedom of Information and Protection of Privacy Act (FIPPA) and other applicable legislation. The College is committed to protecting your privacy and applies best practices in doing so.
For further information regarding privacy considerations, refer to the Pharmacy Licensure Guide.
-
Which applications require submission of a pharmacy diagram? What are the pharmacy diagram requirements and what scale should it be drawn to?
A pharmacy diagram must be submitted for the following change applications:
You must ensure that the diagram is professionally drawn to scale of ¼ inch equals 1 foot. All pharmacies must show that they meet the physical requirements set out in the PODSA bylaws. The diagram checklist (Community or Hospital) will provide a list of all requirements. A diagram that is not drawn to scale or is missing requirements may cause a delay in the application process.
For further information on pharmacy diagrams, refer to the Pharmacy Licensure Guide.
-
How do I complete my pre-opening/change of layout inspection report?
The pre-opening inspection report must be completed as part of the New Pharmacy, Change of Layout, and Change of Location applications. Both items must be submitted:
- Pre-Opening Inspection Report
- Supporting Digital Evidence in the form of photos or videos
Appendix B in the Pharmacy Licensure Guide provides recommended content for digital evidence. If completing a New Pharmacy application or Change of Location application, you must provide digital evidence for all items. If you are submitting a Change of Layout application, complete up to the Security section only.
For further information on the pre-opening inspection, refer to the Pharmacy Licensure Guide.
-
How do I submit photos or video for my pre-opening inspection?
Pre-opening inspections require supporting digital evidence to show your pharmacy meets the requirements for licensure. Digital evidence (photos/videos) may be submitted to the College via email at [email protected] using the PowerPoint template provided by the College or by uploading the digital evidence to a file sharing service such as Google Drive, One Drive, or Dropbox and sharing a link to the folder if the file is too large to transmit via email.
Appendix B in the Pharmacy Licensure Guide provides recommended content for digital evidence on each requirement in the pre-opening inspection report.
For further information on digital evidence, refer to the Pharmacy Licensure Guide.
-
What are some tips for producing the digital evidence?
Digital evidence (photos/videos) is required to show that your pharmacy has met all the physical requirements and that they adhere to the PODSA bylaws. Photos should be taken from a few different angles/distances to provide context. A close-up photo of a physical requirement may not be sufficient; therefore you may need to step back 5-6 feet in order to put the physical requirement in context of its surroundings.
Delays in approving digital evidence are usually due to the following:
- Digital evidence was not provided for all physical requirements
- Context was not provided and the College cannot confirm compliance
- A physical requirement does not meet all descriptive requirements outlined in the PODSA bylaws
Appendix B in the Pharmacy Licensure Guide provides recommended content for digital evidence. If completing a New Pharmacy application or Change of Location application, you must provide digital evidence for all items. If you are submitting a Change of Layout application, complete up to the Security section only.
For further information on digital evidence, refer to the Pharmacy Licensure Guide.
-
My pharmacy is relocating, how do I submit photos to demonstrate compliance when I can’t move my equipment until the day of the move?
A pharmacy that is changing location must meet all of the requirements outlined in the pre-opening inspection report prior to moving into the new pharmacy. The College recognizes that some equipment may still be in use up until the day of the move such as computer terminals, equipment, time-delay safe, fridge, etc. In this case, take photos of the equipment in the existing location and submit a photo showing where the equipment will be placed in the new pharmacy using placeholders. Additional photos may be requested after the move to confirm the final layout of the equipment matches the pharmacy diagram submitted.
-
What is a Central Securities Register and how do I obtain one?
A company/corporation must maintain a Central Securities Register (CSR) in accordance with the requirements in the Business Corporations Act. This document lists the shareholders of the corporation. You can obtain this document from either the lawyer or law firm who incorporated your company, or from the individual who is responsible for maintaining this document within your corporation. This document must include: all shares issued by a company, the name and last known address of each shareholder, and the number, class and any series of any shares owned by that shareholder. This document must be certified by a lawyer or notary before being submitted to the College.
For further information on the Central Securities Register, refer to the Pharmacy Licensure Guide.
-
Can I submit a Register of Directors instead of the Central Securities Register?
No. The Register of Directors only lists the directors and officers of a corporation. In order to validate the names of the shareholders (Indirect Owners) within the corporation, the College requires the certified Central Securities Register which lists the shareholders.
For further information on the Central Securities Register, refer to the Pharmacy Licensure Guide.
-
I am purchasing/selling a pharmacy. What should I do?
The process of purchasing or selling a pharmacy is considered a Change of Direct Owner. This application is submitted to the College by the new Direct Owner of the pharmacy (i.e., the purchaser). However, the current Direct Owner of the pharmacy (i.e., the seller), must confirm the change by signing the application form. The new Direct Owner must submit a Change of Direct Owner application and all applicable requirements to the College at least 30 days before the effective date of change. If updated corporate documents are unavailable 30 days prior to the change, the Deferred Submission of a Required Document(s) for Change Application form must be submitted with the Change of Direct Owner application.
For further information on a Change of Direct Owner application, refer to the College website or the Pharmacy Licensure Guide.
-
What are the differences between a Change of Direct Owner and a Change of Corporation Name?
A Change of Direct Owner occurs when a pharmacy is sold from one entity to another. This also includes amalgamation. A Change of Corporation Name occurs when the corporation that currently owns the pharmacy changes in name only. One way to distinguish the difference is that a Change of Direct Owner will result in a new incorporation number, whereas a Change of Corporation Name will result in the incorporation number staying the same.
For further information, refer to the Pharmacy Licensure Guide.
-
What is the difference between a Direct Owner (DO) and an Indirect Owner (IO)?
The name of the Direct Owner of the pharmacy is printed on the current pharmacy licence. In most cases, the Direct Owner of the pharmacy is a corporation. Indirect Owners of the pharmacy are the directors, officers, and shareholders of this Direct Owner corporation and/or any other corporations related to the ownership structure of this pharmacy. Indirect Owners can be individuals (pharmacists, pharmacy technicians, or non-registrants), or corporations.
- Directors: individuals identified on the Notice of Articles or BC Company Summary, issued by BC Registry Services. The majority of directors of the Direct Owner must be pharmacists. If the directors of a corporation change, you must submit a Change of Indirect Owner application, and the Notice of Change of Directors issued by BC Registry Services.
- Officers: individuals identified on the BC Company Summary or Annual Report issued by BC Registry Services. If the officers of a corporation change, you must submit a Change of Indirect Owner application, and the updated BC Company Summary issued by BC Registry Services.
- Shareholders: any individual or corporation that holds shares of the Direct Owner or Indirect Owner who is identified on the Central Securities Register of a non-publicly traded corporation. If the shareholders of a corporation change, you must submit a Change of Indirect Owner application and an updated certified copy of the Central Securities Register.
Note: If a shareholder is a non-publicly traded corporation, the directors, officers, and shareholders of this corporation are also considered Indirect Owners.
For further information on pharmacy ownership, refer to the College website or the Pharmacy Licensure Guide.
-
What happens if my corporation undergoes an amalgamation?
Amalgamating is the process where two or more corporations merge and carry on as one corporation, the "amalgamated corporation". The “amalgamated corporation” is a new legal entity, regardless of whether the “amalgamated corporation” has the same name or people as any of the “amalgamating corporations”. If the Direct Owner of a pharmacy amalgamates, you must submit a Change of Direct Owner application. An amalgamation is considered a Change of Direct Owner because the “amalgamated corporation” is a new legal entity which has a new BC Incorporation Number.
For further information regarding a Change of Direct Owner application, refer to the College website or the Pharmacy Licensure Guide.
-
My pharmacy is currently undergoing renewal, but I am selling the pharmacy. Should I complete the renewal process or submit a change application? Are the renewal fees refundable?
To maintain a pharmacy licence, either the new Direct Owner must complete the Change of Direct Owner application and its requirements before the existing pharmacy licence expires, OR the current Direct Owner must renew the pharmacy licence before it expires. If the Change of Direct Owner application will not be completed before the pharmacy licence expires, the current Direct Owner should renew the pharmacy licence first. The new Direct Owner can submit the Change of Direct Owner application when the sale is confirmed. If the Change of Direct Owner application is not completed and the current Direct Owner did not renew the pharmacy licence before it expires, the pharmacy must remain closed. The new Direct Owner will then have to apply for a New Pharmacy Licence by following the New Pharmacy Licence process outlined in the Pharmacy Licensure Guide. All licensing fees are non-refundable.
Note: If the current Direct Owner will not be renewing the pharmacy licence, the new Direct Owner must inform the College of the Change of Direct Owner by submitting the Change of Direct Owner application before the pharmacy renewal deadline, i.e., 30 days before the licence expires. If all requirements for the pharmacy renewal application are not submitted before the deadline, and the College has not been informed of the Change of Direct Owner via an application, then the renewal is considered late and will be referred to the Application Committee for review and an administrative fee may be applied.
For further information regarding a Change of Direct Owner application, refer to the College website, or the Pharmacy Licensure Guide.
-
I only hold non-voting shares of the Direct Owner or corporation associated with the ownership of a pharmacy. Am I still considered an Indirect Owner and required to submit Proof of Eligibility?
Yes, all shareholders, regardless of the type or number of shares they hold, are considered Indirect Owners of the pharmacy and must submit Proof of Eligibility for all applicable applications.
For further information on Indirect Owners and pharmacy ownership, refer to the Pharmacy Licensure Guide.
-
I’m not a registered pharmacist in BC. Can I own a pharmacy?
Yes, non-pharmacists may have ownership of a pharmacy. However, the majority of directors of the Direct Owner must be pharmacists registered in BC. In order to meet the majority requirement, more than 50% of the directors must be pharmacists (regardless of who has the majority of shares within the corporation).
Note: All Direct Owners and Indirect Owners must also comply with the eligibility criteria outlined in the Pharmacy Operations and Drug Scheduling Act. One of the criteria to hold a pharmacy licence is that “a person authorized by an enactment to prescribe drugs must not be a Direct Owner or an Indirect Owner.”
For further information on pharmacy ownership, refer to the Pharmacy Licensure Guide.
-
Where can I take my English Language Proficiency (ELP) test?
Refer to Appendix 1 of the Registration Committee Policy-1 for a list of the accepted ELP assessments.
-
How often is the Jurisprudence Exam (JE) held?
JE sittings are held three times a year in February, June and October. Refer to the College website for details. This webpage will be updated when the exam date, times and locations have been confirmed.
-
I am registered in another province as a pharmacist or pharmacy technician and am applying through the “Canadian Free Trade Agreement” (CFTA). Do I need to write the BC Jurisprudence Exam?
No. As a registered, practicing pharmacist or pharmacy technician from another Canadian province/territory, you are not required to complete any additional assessments, including the BC Jurisprudence Exam.
-
What is the validity period of my Jurisprudence Exam (JE) results?
JE results are valid for 3 years from the date the exam was written.
-
When does the registration for the next sitting of the Jurisprudence Exam (JE) open and close?
JE registration opens online approximately two months before the exam date and closes approximately one month before the exam date. Once the exam date, times and locations have been confirmed, the College website will be updated. You can also find the registration deadline date on the same webpage.
-
Can the hours that I completed for my practicum as part of my pharmacy technician program be applied towards a reduction in my Structured Practical Training (SPT) hours?
No, because the hours completed during your program has already been taken into account.
-
How long does it take to process my pharmacy technician Structured Practical Training (SPT) application?
When received, up to 5 business days. Once completed, a confirmation email will be sent.
-
Can I email or fax my pharmacy technician Structured Practical Training (SPT) application?
Yes, you can email or fax it to the College.
-
Do I get paid for my pharmacy technician Structured Practical Training (SPT)?
Whether or not you are paid during your SPT, is an arrangement that is made between you and your site. The College is not involved with this arrangement.
-
How long does it take to process my Drug Administration Certification application?
When received, up to 5 business days. Once completed, a confirmation email will be sent.
-
When can I submit my registration renewal application?
You can complete your registration renewal once you have received your renewal notice, which is sent via email approximately 6 weeks before your registration expiry date. You will not have access to submit your registration renewal application on eServices prior to receiving the renewal notice and fulfilling your CE requirements. Refer to the Registration Renewal section on the College website for details on the renewal process.
-
When is the latest I can submit my registration renewal application?
You have up to the registration expiry date to submit your renewal application. The College recommends that you submit it as soon as possible upon receipt of the notice. Try to avoid submitting it on the last day, especially if it is during the weekend, as the College will be unable to provide you support if you experience any technical issues when the office is closed.
-
How do I get my employer to pay for my registration renewal?
You need to submit your online registration renewal application through eServices first, which includes the completion of your declarations (Statutory declaration, Professional Liability Insurance and Drug Administration re-certification, if applicable). When you reach the “Summary” tab, you will see a link to print the invoice to give your employer. The employer can then mail the payment (cheque, bank draft or money order) along with this invoice or phone the College office to provide their credit card information (Visa or Mastercard). Please note, Visa debit cards are not accepted.
If payment is not received, your registration renewal is incomplete. It is a registrant’s responsibility to ensure payment is received at the College by their renewal due date.
-
I am in the process of renewing my registration and am trying to update my employment information. I work as a relief pharmacist only so how do I enter this information?
You need to list all the pharmacies where you provide relief coverage as your place of practice and select the pharmacy where you work the majority of time as your primary place of practice. Do not choose your corporation (head office) as your primary place of practice.
-
I am trying to renew my registration but cannot move past the employment page. What can I do?
When using eServices, using a supported browser is recommended to ensure the best results. Please note that mobile devices such as smart phones, tablets and iPads are not supported. It is also important to ensure you have the most recent version of the web browser installed on your computer. Supported browsers for eServices include:
- Internet Explorer 8-11 (IE Edge not recommended)
- Google Chrome
You can also try clearing your cache/browsing history:
- For Steps to clear your browser history in IE
- For Steps to clear your browser history in Chrome
Contact the Registration Department if you need further assistance.
-
If I am not currently working in BC, do I still need to have professional liability insurance?
Yes. Registrants must maintain at all times professional liability insurance coverage while registered as a Full Pharmacist or Pharmacy Technician, regardless of whether or not you are currently working in BC, as it is tied to the registration class. As indicated in renewal requirement #6 on the College website, your professional liability insurance must meet the following 3 criteria:
- Provides a minimum of $2 million coverage.
- Provides occurrence based coverage or claims made coverage with extended reporting period of at least 3 years.
- If not in the pharmacists’ or pharmacy technicians’ name, the group policy covers the pharmacist or pharmacy technician as an individual
-
How can I get a certificate of standing?
Place an order through eServices by clicking Events & Services > Online Store and then choose “Certificate of Standing”. When placing the order, enter instructions and/or the name and address of the regulatory authority where it needs to be sent in the “Order Instructions” field. It takes 5-10 business days to process the order once received.
-
How can I get a copy of my receipt related to registration (for applications, renewal fees, online purchases, etc)?
All receipts are available through eServices under My Profile > My Receipts.
For renewal fees, if you also paid the $28 fee Criminal Record Check fee, it is on a separate receipt so scroll down the PDF to see the second page.
-
I would like to change to the non-practising class before I am due for renewal. How do I change my registration class?
To register as a Non-Practicing pharmacist, you must transfer directly from the Full Pharmacist register to the Non-Practicing Pharmacist register at the time of your next renewal.
-
How Do I Create the Pharmacy Professionals Review Schedule?
It is the pharmacy manager’s responsibility to schedule individual Pharmacy Professionals Reviews for all registered pharmacists and pharmacy technicians employed at their site.
To create the Pharmacy Professionals Review schedule, the pharmacy manager should refer to the existing staff schedule, the staff roster, as well as the Pharmacy Professionals Review Scheduling Template provided by the College in the selection email. The pharmacy manager can simply plug in names to the College template and send a copy to the PRP Coordinator as soon as it is complete and no later than two weeks prior to compliance officers arriving on-site.
-
If a learning activity was accredited at the time I completed it and the accreditation is now expired, can I still document it as accredited learning?
Yes, if the learning activity was accredited at the time you completed it, you can document it as accredited learning. Learning activities must occur within the last year (past 12 months) of your renewal date to be considered current.
-
If I complete more than the minimum hours of accredited learning activities for my current yearly renewal, can I use the additional accredited hours for my next renewal?
No, the completion date of the learning activities must occur within the 12 months prior to your individual renewal date, even though the accreditation is still valid (not expired) beyond that date.
-
What is a Learning Record?
A Learning Record is an online form that assists you in documenting your learning activities. Registrants must complete and submit a minimum of 15 hours of learning documented on a minimum of 6 Learning Records prior to registration renewal each year, if they are renewing registration as a full registrant. A minimum of 5 hours must be accredited learning and supporting documentation needs to be provided as part of the Learning Record(s) it pertains to. Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
Can I put all my 6 learning goals and activities for the year on one learning record?
No, you must identify, fill out and submit at least 6 separate Learning Records - one for each goal - every year. Individual learning activities that you have undertaken during the year can be combined based on the goal and documented on one of these 6 Learning Records. You must have a minimum of 15 hours of learning documented on a minimum of 6 Learning Records. A minimum of 5 hours must be accredited learning and supporting documentation needs to be provided as part of the Learning Record(s) it pertains to. Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
If I have more than the minimum hours and/or Learning Records, can I use the additional hours/Learning Records for my next renewal?
No, hours and Learning Records cannot be carried over from year to year. Learning has to take place within the 12 months prior to your individual renewal date.
-
Do I have to complete my Continuing Education (CE) before I can pay for my renewal for the next year?
Besides CE, there are many other requirements for renewal, including payment. You can begin the renewal process at any time, but in order to complete the renewal process, including payment, you must have completed and submitted your CE requirements for the most recent 12 months of your registration renewal date.
-
Do CEU’s (Continuing Education Units) count?
Continuing Education Units (CEUs) are assigned by the accrediting body to a specific learning activity. The “conversion” of CEUs into accredited hours varies between different accrediting bodies; the requirement is for accredited hours. You should confirm with the course provider the number of hours the activity is accredited for.
-
Does out of country learning count?
Yes, learning from any source is acceptable as long as it is within your scope of practice as a pharmacist or pharmacy technician.
-
What happens if I do not complete all the requirements by my renewal date?
If you do not renew your registration by the registration expiry date, you will no longer be registered with the College and will become a “former” registrant. This means that you will not be a registered pharmacist or pharmacy technician in BC, you will not be allowed to practice pharmacy in BC and your access to PharmaNet will be terminated. If you are also a manager of a pharmacy, your pharmacy licence will be cancelled. If you wish to become a registrant again, you will have to complete the reinstatement process applicable to your registration class (pharmacist or pharmacy technician) and pay applicable fees.
The specific reinstatement requirement depends on the time period lapsed between your registration expiry date and the time you apply for full registration. Your Continuing Education submissions for reinstatement will require up to 5 business days to review; you will be advised via email of their status, or if additional information is required. More information can be found here.
-
What are my Continuing Education (CE) requirements for registration renewal?
To fulfill your CE requirements for renewal, you must:
- successfully complete at least 15 hours of learning activities documented on a minimum of 6 Learning Records of which a minimum 5 hours must be accredited learning, (supporting documentation needs to be provided as part of the Learning Record(s) it pertains to). Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
- complete all learning activities in the most recent 12 months of your registration renewal date
- successfully complete at least 15 hours of learning activities documented on a minimum of 6 Learning Records of which a minimum 5 hours must be accredited learning, (supporting documentation needs to be provided as part of the Learning Record(s) it pertains to). Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
If I am renewing as a non-practicing registrant, do I still need to complete Continuing Education (CE)?
No. CE is only required for registrants that are renewing registration as a full registrant.
-
If I am planning to become a former registrant, do I still need to complete Continuing Education (CE)?
No. CE is only required for registrants that are renewing registration as a full registrant.
-
Are the Continuing Education (CE) requirements for Registration Renewal different for pharmacists and pharmacy technicians?
No. The CE requirements are the same for both pharmacists and pharmacy technicians that are renewing their registration as a full registrant.
-
Can all my Learning Records/Activities be accredited learning?
Yes, all learning can be accredited as there are no minimum requirements for non-accredited learning.
To fulfill your Continuing Education (CE) requirements for registration renewal, you must:
- successfully complete at least 15 hours of learning activities documented on a minimum of 6 Learning Records of which a minimum 5 hours must be accredited learning, (supporting documentation needs to be provided as part of the Learning Record(s) it pertains to). Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
- complete all learning activities in the most recent 12 months of your registration renewal date
- successfully complete at least 15 hours of learning activities documented on a minimum of 6 Learning Records of which a minimum 5 hours must be accredited learning, (supporting documentation needs to be provided as part of the Learning Record(s) it pertains to). Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
How do I “Submit” more than the minimum requirements?
You can “Submit” your Learning Records one by one, as you complete them, or you may choose to “Submit” them all at once.
If you “Submit” the Learning Records one by one, once the minimum requirements have been satisfied, you will not be able to “Submit” additional Learning Records. You can record and “Complete” further Learning Records, however, they cannot be “Submitted”.
If you “Submit” the Learning Records all at once, then you can “Submit” more than the minimum requirements.
-
What if I spend more time on a learning activity than what it is accredited for?
Document the hours the activity is accredited for under the “Accredited Hours” field. Any additional time spent beyond what the activity is accredited for, can be recorded as “Non-Accredited Hours” using increments of 0.25 hours (15 minutes).
-
What supporting documentation should I submit along with my Learning Records?
For accredited learning:
Uploading supporting documentation including certificates, letters of completion, or school transcripts is required to provide confirmation of successful completion of accredited learning activity.
Supporting documentation with your name, the accrediting body, the number of accredited hours assigned, the date of completion, date accreditation is valid until, is issued by the course provider. If unsure, confirm with the course provider. Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
For non-accredited learning:
Uploading supporting documentation is not required for non-accredited learning. You may choose to upload a photocopy of the cover of your reading material, flyer advertising an event you attended, an email verifying a meeting or conversation for your own record-keeping purposes.
-
What should I do if my Learning Records are not counting towards my minimum Continuing Education (CE) requirements?
Please ensure that you have “Submitted” your Learning Records as only “Submitted” Learning Records “count” towards satisfying your CE requirements. A Learning Record may be:
- In Progress: required information is missing from specific fields. Learning Record cannot be “Submitted”.
- Complete: all required information has been entered. Learning Record can be “Submitted”.
- In Progress: required information is missing from specific fields. Learning Record cannot be “Submitted”.
-
What is the minimum amount of time I can record for a learning activity?
You can record activities in 0.25 hours (15 minutes) increments, with the shortest activity being 0.25 hours.
-
How do I access Learning Records from previous cycle years on the PDAP Portal?
Once you are logged in to the PDAP Portal, click on “Complete Learning Records” then under “Select Renewal Year to view” and choose your desired cycle year from the drop down menu. The portal will display the Learning Records for that cycle year.
-
How do I “Submit” my Learning Records on the PDAP Portal?
You can “Submit” your Learning Records one by one, as you complete them, or you may choose to “Submit” them all at once.
Select the Learning Record(s) you wish to “Submit” by clicking on the box(es) on the left hand side and press “Submit”.
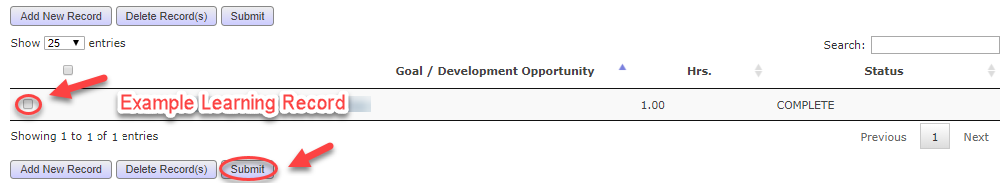
-
How do I know if I have completed all the requirements?
The following will be displayed on your device screen once the continuing education (CE) requirements have been satisfied.
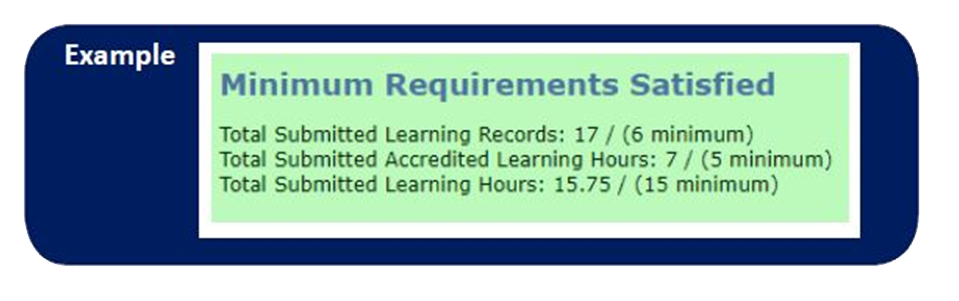
-
I have just received a prescription with the following statement “Do Not Renew &/or Adapt” (or something similar) hand-written on it. Does this mean that I cannot adapt or renew this prescription?
Yes. Just like we honour notations like this from prescribers today regarding generic substitution pharmacists are expected to honour hand-written “Do Not Renew &/or Adapt” instructions on prescriptions. The College of Physician and Surgeons (CPSBC) have agreed that pre-printed prescription pads are not acceptable and if a physician electronically produces their prescription they must sign or initial beside the notation.
It is important to remember that should a pharmacist, presented with a valid notation on a prescription, still feel that an adaptation or renewal is in the best interest of the patient there are a number of options still available to them: contact the prescriber or provide an emergency fill (PPP-31) to ensure continuity of care giving the patient time to get in to see their physician.
-
I just received a request for a prescription transfer from a pharmacist in Seattle, Washington. May I transfer the prescription?
According to the Health Professions Act - Bylaws Schedule F Part 1, upon request a pharmacist must transfer prescriptions to another pharmacy licensed in Canada, if the drug does not contain a controlled drug substance and the transfer occurs between a registrant and another registrant or an equivalent of a registrant in another Canadian jurisdiction. The Bylaw does not address transferring a prescription to the U.S. In the interest of positive patient outcomes registrants may use professional judgement and decide to transfer a prescription to a state that is allowed to accept transfers from Canada. However, once the prescription is transferred out of B.C. the pharmacy is not allowed to transfer the unused refills back to B.C.
-
I have a patient with cancer who wants to receive medical marijuana. What does the patient need to do to?
Medical use of cannabis is federally regulated by Health Canada. Please visit this link for more information: https://www.canada.ca/en/health-canada/topics/cannabis-for-medical-purposes.html
-
How will scheduling work?
Every pharmacy will be reviewed cyclically on a multi-year time frame. The College will be looking at a number of factors when scheduling reviews.
The College will confirm a date for the Practice Review with feedback from the pharmacy manager. It is the pharmacy manager’s responsibility to ensure that their staff are available during the scheduled Practice Review.
-
What should I do if I have satisfied the CE requirements on the PDAP Portal but see a message saying “You must satisfy your Continuing Education (CE) Requirements in order to complete your Registration Renewal.” when I try to renew registration?
Please contact the PDAP Department: (604) 733-2440, or email us at: [email protected] for assistance.
-
When should I submit my pharmacy change application? How much notice do I need to give the College?
Pursuant to section 4 of the Pharmacy Operations General Regulation, the College must be notified as follows:
“(a)at least 7 days before a manager ceases to manage a pharmacy;
(b)at least 30 days before the location of a pharmacy changes;
(c)at least 30 days before a direct owner changes;
(d)at least 7 days before an indirect owner changes;
(e)on becoming aware that a direct owner has ceased to be eligible, under section 3 of the Act, to hold a pharmacy licence.”Additionally, pursuant to section 4.1(3) of the Pharmacy Operations and Drug Scheduling Act (PODSA):
“a direct owner must give to the registrar 30 days' written notice of any changes respecting the name or layout of the pharmacy.”
Pursuant to section 18(8)(d) of the PODSA Bylaws, a pharmacy closure application must be submitted at least thirty days before the effective date of proposed closure.
Failure to submit an application within the correct timeline may lead to a delay in the application process or referral to the Application Committee.
A summary of the prescribed timelines for all pharmacy applications can be found in the Pharmacy Licensure Guide.
-
Why do I have to submit a Criminal Record History (CRH) for the pharmacy application? I have already completed a Criminal Record Check (CRC) during my pharmacist registration renewal. What is the difference between the two checks?
All registered pharmacists and pharmacy technicians currently undergo a CRC through the Criminal Records Review Program (CRRP) as required under the Health Professions Act (HPA) at the time of initial registration and at least every 5 years thereafter at the time of registration renewal. This CRC check only reviews selected offences under the Criminal Code, whereas the CRH reviews all the convictions under the Criminal Codes within the previous 6 years. The CRRP is also specific to registrants and does not provide a means for the CRH of non-registrants to be checked.
The College cannot use the same CRC under the CRRP for the pharmacy licensure process since it does not meet the CRH requirements in PODSA.
All Direct and Indirect Owners and managers must submit a CRH as part of the licensure process. All owners who are registered pharmacists and managers must continue to undergo the separate CRC process to maintain their registration with the College.
For further information on the differences between CRC and CRH, refer to the Pharmacy Licensure Guide.
-
What do I need to provide for my pre-registration and full registration applications?
Use the following checklists to help you collect all requirement documents for your application:
- Application Checklist for Pre-Registration/Student Pharmacist Registration
- Application Checklist for Full Pharmacist/Pharmacy Technician Registration
Also review the College’s Scanning Guidelines and Checklist for Document Submissions and ensure your documents meet the requirements.
-
Who can notarize my documents?
Only a notary public or lawyer will be accepted for notarizing your documents. Other professionals, including a Commissioner for Oaths, will not be accepted.
-
How long does it take to process my pre-registration application?
It takes at least 45 days to process the application due to the Criminal Record Check (CRC). If adjudication or fingerprinting is requested by the Ministry of Public Safety and Solicitor General, the processing time will be delayed. Once your application has completed processing, you will receive a confirmation email.
-
How should I submit my application documents?
Documents for your pre-registration and full registration applications should be uploaded through the online application modules unless otherwise instructed. Ensure documents are scanned in accordance with the College’s Scanning Guidelines and Checklist for Document Submissions. Fax will not be accepted.
-
Some of my documents are not in English, will they be accepted?
Documents in a language other than English must be translated by a certified translator. Thus, documents that require notarization, should be notarized first and then translated.
-
I am an International Pharmacy Graduate. Will my pharmacy degree be accepted in Canada?
Contact the Pharmacy Examining Board of Canada (PEBC) to have your documents evaluated. Visit the PEBC website (www.pebc.ca) for more information.
-
I will be starting first year in the pharmacy program at UBC. By when do I need to submit my student registration?
Your online student registration application and notarized documents should be received by the College office no later than September 1, before the start of your first year in the pharmacy program.
-
I am currently working as a pharmacy assistant. Is the Pharmacy Technician Bridging Program (PTBP) still available to get registered as a pharmacy technician?
The PTBP is no longer available for pharmacy assistants to become registered in BC as a pharmacy technician. To become a pharmacy technician in BC you will need to take the New Pharmacy Technician Graduate path and successfully complete a CCAPP accredited pharmacy technician program offered through a public or private college: https://www.bcpharmacists.org/new-pt-graduate-canada.
-
How long does it take to process my reinstatement application?
It takes at least 45 days days to process the application due to the Criminal Record Check (CRC). If adjudication or fingerprinting is requested by the Ministry of Public Safety and Solicitor General, the processing time will be delayed. Once your application has completed processing, you will receive a confirmation email..
-
Can I email my reinstatement application and documents?
Yes, they can be mailed or emailed as long as the documents meet the requirements outlined in the College’s Scanning Guidelines and Checklist for Document Submissions. Fax will not be accepted.
-
How long does it take to process my full registration (Pharmacist or Pharmacy Technician) application?
Once you have submitted your application, it will be reviewed within 5 business days. Any changes or updates (including the addition of PEBC certification results) made to your application will require up to 5 business days to review. You will be notified by email of any updates to your application status.
Full registration applications are generally submitted online through eServices, although a paper application will be required for specific scenarios. If the latter, instructions will be provided to the applicant. You will be notified by email:
- If any required documents are rejected or missing;
- When there is an update to your application including instructions for submitting payment to complete your full registration;
- When your application is complete.
If any updated documents are required for your full registration application, most documents can be uploaded directly to the Full Registration online system unless otherwise instructed. These documents must be scanned in accordance with the requirements outlined in the College’s Scanning Guidelines and Checklist for Document Submissions document. Submitted documents will be rejected if they do not meet the scanning requirements.
-
Can I email or fax my Full Registration application?
If you were provided with instructions to complete a paper application for your Full Registration, you may submit it by email. Otherwise, all other Full Registration application must be completed online through eServices. Log into your eServices account and select “Full Registration” after your pre-registration application is processed and you have completed all other registration requirements.
-
Where can I obtain professional liability insurance?
Professional liability insurance may be provided by an employer or purchased yourself through a private insurance broker or membership with the BC Pharmacy Association. Your insurance must meet the three criteria listed on the Professional Liability Insurance for Pharmacy Professionals section of our website.
-
I was born and raised in Canada, and completed high school in Canada but I received my pharmacy degree in the United Kingdom. Do I still have to complete an English Language Proficiency (ELP) assessment?
Yes. According to the ELP standards set by the National Association of Pharmacy Regulatory Authorities (NAPRA), if you obtained your pharmacy degree outside of Canada or the USA, you are required to complete an English Language Proficiency assessment, regardless of your previous secondary or post-secondary education, work experience, or official language of the country where you obtained your pharmacy degree. Please refer to the Registration Committee Policy-1 on the College website.
-
How can I submit my English Language Proficiency (ELP) assessment scores?
Official ELP results must be sent directly from the testing agency to the College. However, for IELTS and TOEFL, a copy of the score report or the IELTS TRF number is accepted via email or fax from an applicant because IELTS and TOEFL scores can be verified online.
-
What is the validity period of my English Language Proficiency (ELP) result?
ELP results are valid for 2 years from the date the exam was written. ELP results must be valid at the time that you begin your practical training for the Structured Practical Training (SPT) requirement.
-
How can I register for the Jurisprudence Exam (JE)?
Registration for the JE is completed online through eServices.Thus an applicant must be pre-registered with the College or registered as a student pharmacist in the final year of the pharmacy program at UBC, to be eligible to write the JE.
-
What is being tested in the Jurisprudence Exam (JE)?
The JE is based on legislation contained in federal and provincial acts, their regulations, bylaws and published College Professional Practice Policies that pertain to pharmacy practice and registrant (pharmacist or pharmacy technician) responsibilities in the practice of pharmacy. Refer to the JE Information Guide for details.
-
For pharmacist registration, where/how do I complete Structured Practical Training (SPT)?
If Structured Practical Training (SPT) is required, it is completed through the Canadian Pharmacy Practice Program (CP3) at UBC’s Division of Continuing Pharmacy Professional Development. The College recognizes the SPT component within the CP3 program as fulfilling the SPT requirement for the College. Full program enrollment is required. Please contact UBC for any questions regarding the CP3 program.
-
For pharmacist registration, how many hours of Structured Practical Training (SPT) am I required to complete?
Pharmacist applicants who are required to complete the SPT are required to complete 500 hours. Please refer to Registration Committee Policy 6 for the types of applicants who are required to complete SPT
-
How do I obtain a work permit?
The College does not provide information regarding work permits. Contact Immigration, Refugees and Citizenship Canada (IRCC) directly for details regarding work permits.
-
For pharmacy technician registration, how many hours of Structured Practical Training (SPT) am I required to complete?
Pharmacy technician applicants are required to complete 160 hours of SPT, if they graduated within the last 3 years preceding their SPT start date, or 500 hours of SPT if they graduated 3 years or greater preceding their SPT start date. Please refer to Registration Committee Policy 8 for details.
-
What is the validity period of my pharmacist or pharmacy technicians Structured Practical Training (SPT) result?
SPT results are valid for 3 years from the date of completion.
-
Can I email or fax my Drug Administration Certification application?
Yes, you can email or fax it to the College.
-
I have received my registration renewal notice but it won’t allow me to renew as it is showing an error message that states my CE’s are not complete.
You must complete your CE requirements before you can renew. If you have completed your CE requirements but see the error message that you have not completed them, contact the Professional Development Department at: [email protected].
-
What are the consequences if I do not renew on time?
You will be transferred to the Former registrant category. As a Former registrant, you will not be permitted to practice pharmacy in B.C. and your access to PharmaNet will be disconnected. Your Drug Administration Certification (if applicable) will also be removed and you will be required to re-apply.
Please note that you will still have access to eServices to complete your renewal, for up to 90 days from your expiry date. However, a late fee will be applied as per HPA Bylaw Schedule D – Fee Schedule.
-
I am trying to update my employment information but I cannot find my place of practice in the system?
All BC licensed pharmacies can be found in the system. For all others, enter the name and address of your place of employment in the “Other Employer” text box in eServices. The Registration Department will review the information, add your employer to the list, if applicable or they will contact you for further information.
-
I just renewed my registration, where can I get my new registration card?
You can print out your new wallet-size registration card through eServices under “My Profile” only when your current one expires because eServices is in real time. For example, if a registrant completes their renewal before their renewal due date of October 31st, then the new card will be available on November 1st.
-
I am certified for Drug Administration but I am not currently providing any immunizations via injection or intranasal route because I am in the processing of recertifying my First Aid/CPR as it has recently expired. Is that acceptable?
No, you must maintain at all times valid First Aid and CPR certification throughout your Drug Administration Certification and not let it lapse, otherwise your Drug Administration Certification will no longer be valid. To become certified again, you may be required to re-complete a CCCEP-accredited drug administration training course and/or First Aid & CPR certification course. If you wish to acquire your drug administration certification again, email the Registration Department at: [email protected], immediately for the re-certification requirements. Refer to renewal requirement #7 on the College website.
-
How do I renew my Drug Administration Certification?
Your Drug Administration Certification must be renewed each year at the time of your registration renewal. You will be required to declare if you meet all three Drug Administration renewal requirements below:
- In the preceding three years, administered a drug via injection route or successfully completed a continuing education program in drug administration as specified in Schedule C, and
- In the preceding three years, administered a drug via intranasal route or successfully completed the Intranasal Administration Online Module as specified in Schedule C, and
- Maintained valid First Aid and CPR certification throughout their drug administration certification as specified in Schedule C.
If you do not satisfy all three requirements to complete the drug administration renewal declaration, your certification will no longer be valid. To become certified again, you may be required to re-complete a CCCEP-accredited drug administration training course and/or a First Aid & CPR certification course. If you wish to acquire your drug administration certification again, email the Registration Department for the re-certification requirements.
-
How often do I need to do my Criminal Record Check (CRC)?
The CRC is completed for all registrants at least once every 5 years. Thus, a new CRC is initiated in the 4th year because it must to be completed before you exceed the 5 year mark. Further details can be found on the College website.
-
I just had a Criminal Record Check (CRC) done for my volunteer work. Do I have to complete another CRC for the College?
Yes, we require a separate CRC to be conducted, as the CRC for your registration must be initiated through the College and completed by the Ministry of Public Safety and Solicitor General.
-
I just completed a Criminal Record Check (CRC) for my registration renewal and I am applying to do some volunteer work. Can the College forward a copy of my CRC to another organization?
The College does not receive any specific details regarding the CRC. We only receive confirmation of whether your CRC is cleared or not. However, you can inquire directly with the Ministry of Public Safety and Solicitor General about sharing the details and results of your criminal record check with other organizations.
-
I just had a Criminal Record History (CRH) done for my pharmacy licence renewal application (as I am the manager/indirect owner of a pharmacy). Do I have to complete another Criminal Record Check (CRC) for the College?
Yes, the CRC required for your registrant renewal is different from the CRH for your pharmacy renewal. They are required for different purposes under two different pieces of legislation.
The CRH is required for all pharmacy managers and direct/indirect owners of a pharmacy for pharmacy license applications under the Pharmacy Operations and Drug Scheduling Act. The CRH is processed by Sterling Backcheck, results are sent to the College and reviewed by the College's Application Committee, if required.
The Criminal Codes reviewed for the CRC and CRH are not the same, and therefore, are not interchangeable. The CRC is specific to registrants and is not applicable to pharmacy owners that are not registrants. As such, all direct and indirect owners and managers must submit a CRH as part of the licensure process.
-
How long is my Certificate of Standing valid for after submitting my Pre-Registration application?
If an applicant does not complete the requirements for full registration within 12 months from the date the pre-registration application was received, an updated certificate of standing is required. Please refer to the Health Professions Act bylaws (Section 42(1.1)) on the College website.
-
What are the requirements of my Certificate of Standing for my Pre-Registration application?
A Certificate of Standing must be mailed or emailed directly from the regulatory body(ies) to the College office and dated no earlier than 3 months from the date the pre-registration application was received.
-
When do I receive my Registration Certificate after completing my Full Registration?
A Registration Certificate will be mailed to the mailing address in your eServices account approximately 8 weeks after completing your Full Registration.
-
How do I order a replacement registration certificate?
Place an order through eServices by clicking Events & Services > Online Store and then choose “Replacement of Registration Certificate”. The College requires the original certificate to be returned to the College before a replacement certificate can be printed. However, if your certificate is lost, a notarized affidavit must be mailed to the College. The affidavit should state that you no longer possess the initial registration certificate you received because it is lost, and if the initial certificate is found, you must return one of the certificates to the College.
-
What registration classes are in legislation?
All registration classes are listed in section 41 of the HPA Bylaws, and individuals who are registered in any of those classes are collectively referred to as “registrants”. The College currently has 10 registration classes, which can be grouped into 4 major types:
- Full Pharmacist or Pharmacy Technician
- May practice pharmacy to their full scope of practice in British Columbia
- Annual registration fee required
- Professional liability insurance required
- Professional Development and Assessment Program (PDAP) requirements must be completed for annual registration renewal
- Non-Practicing Pharmacist or Pharmacy Technician
- May use the title “Pharmacist (Non-Practicing)” or “Pharmacy Technician (Non-Practising), but must not provide pharmacy services in British Columbia
- Annual registration fee required
- Professional liability insurance not required
- PDAP requirements not required for annual registration renewal
- Must apply for reinstatement to transfer back to the Full Pharmacist or Pharmacy Technician category and to provide pharmacy services
- This registration class is not available for initial registration with the College. A Full Pharmacist or Pharmacy Technician may transfer to this class at registration renewal.
- Limited Pharmacist or Student Pharmacist
- May provide pharmacy services only under the supervision of a Full Pharmacist, as they have not met all requirements for full registration.
- Registration can be renewed twice for a maximum of three years for Limited Pharmacists; registration must be renewed annually until graduation for UBC students but no renewal for non-UBC students.
- Annual registration fee is required for Limited Pharmacists.
- Professional liability is required for Limited Pharmacists.
- PDAP requirements not required for annual registration renewal.
- Student Pharmacist registration is ceased at graduation. Pharmacy students who have graduated from their pharmacy program but wish to continue providing pharmacy services under the supervision of a Full Pharmacist may apply for Limited Pharmacist registration after graduation, if eligible.
- Limited Pharmacist registration application must be reviewed by the Registration Committee.
- Temporary Pharmacist or Pharmacy Technician; Temporary Limited Pharmacist; Temporary Student Pharmacist
- Temporary registration is only enabled under 45(1) of the HPA Bylaws.
- Differences for each class can be found here: https://www.bcpharmacists.org/temporary-registration
For those who are not registered in any of the above classes, they are not a registrant and are termed a Former Pharmacist or Pharmacy Technician if they were registered as a Full Pharmacist or Pharmacy Technician with the College at one time.
- Must not provide pharmacy services and cannot use the reserved title “Pharmacist” or “Pharmacy Technician”
- Annual registration fee not required
- Professional liability insurance not required
- PDAP requirements not required
- Must apply for reinstatement to transfer back to the Full Pharmacist or Pharmacy Technician category and to provide pharmacy services
- May order Letter of Standing and replacement of Registration Certificate.
- Full Pharmacist or Pharmacy Technician
-
I am not practising now as I am currently on leave. Should I change to non-practising? Or do I have to change to Former?
It is up to a registrant whether or not they choose to renew and maintain their registration in the same registration class or transfer to Former while on any type of leave of absence. For complete details on the registration renewal requirements, refer to the College website. If a registrant chooses not to renew their registration and decides to transfer to the “Former” category upon their next renewal, they can do so by logging into their eServices account to submit a transfer request online. Click on Renew Registration > Former > Proceed to Renewal.
Registrants who are unemployed or on leave are not required to transfer to the non-practising registration class, which is generally intended for those who do not provide pharmacy services (direct-patient care) but chooses to maintain registration for keeping the “pharmacist (non-practising)” title for work purposes or meeting the pharmacy ownership director requirements. Registrants who decide to change to non-practising are expected to understand their responsibilities should they wish to reinstate their registration to Full Pharmacist and Pharmacy Technicians in the future.
Registrants who transfer to the “Former” or “Non-Practicing” categories will have to apply for reinstatement and complete all reinstatement requirements before they can be transferred back to the Full Pharmacist or Pharmacy Technician registration class. At least 45 days is required to process the Reinstatement application due to the Criminal Record Check (CRC) and up to 5 business days to process the Full registration application. Refer to the College website for details on the Reinstatement process in the “Less than 6 years in Non-Practicing or Former” category and “6 years or more in Non-Practicing or Former” category.
-
Can I use professional liability insurance coverage obtained in another province to meet BC requirements?
This depends on whether the professional liability coverage you have covers activities in BC. If the professional liability insurance coverage obtained in another province covers your activities in BC, then you may use it to meet the CPBC registration requirements.
If the coverage you have obtained does not cover your activities in BC, then you will be required to purchase new or additional professional liability insurance to meet the CPBC registration requirements.
-
Can I use the professional liability insurance coverage I have in another country to meet CPBC registration requirements?
The coverage obtained in another country will likely be restricted to the work performed in that country. You will need to confirm whether your insurance coverage extends to BC.
-
I am not registered as a Student Pharmacist nor Non-Practising Registrant. Do I need to have professional liability insurance even though I am not currently working?
Yes, professional liability insurance is required if you wish to maintain your registration. The requirement is determined by your registration class, not by whether you are actively practising or providing pharmacy services to patients in BC.
This applies to registrants on any type of leave of absence, including parental or medical leave, who wish to maintain their registration.
-
What do I do when my first aid and CPR has expired and I cannot complete my first aid and CPR recertification until a later day?
Your drug administration certification (DAC) becomes invalid until recertified. You must not administer any drugs by injection or intranasal route immediately; otherwise, you will be engaging in authorized practice. You must inform the College immediately to remove your DAC.
Once you have obtained your first aid and CPR recertification, contact the Registration Department. You may resume administering drugs by injection or intranasal route once you have successfully recertified your DAC.
-
Is it within a pharmacist’s scope to apply patches that contain medication on a patient, if requested?
Pharmacists are permitted to apply medicated patches on a patient, if requested to do so. However, prior to performing this activity, the pharmacist must ensure that they have the knowledge, skills and abilities to apply the patch in a manner that is safe and appropriate. The pharmacy would also be expected to have policies and procedures in place regarding this activity, including but not limited to, addressing how patients’ privacy needs will be met.
-
Do I have to adapt a prescription?
No. Authorization does not mean obligation. The decision to adapt a prescription or not is at the discretion of the individual pharmacist. Whenever a pharmacist chooses to adapt a prescription however, the adaptation must be done in accordance with PPP-58 and within the limits of the pharmacist’s own competencies.
-
Can I provide a renewal for narcotic, controlled drug or targeted substance under PPP-58?
Yes, but only if permitted under a section 56 exemption to the Controlled Drugs and Substances Act. The pharmacist may use their professional judgement to determine if they have the appropriate knowledge and if it is in the patient’s best interest to do so. If they are comfortable with their assessment, they can make the decision to provide an adapted renewal of a narcotic, controlled drug or targeted substance for a duration up to, but not exceeding, the duration originally prescribed.
This only applies to adapted renewals. A pharmacist must not perform other adaptations on narcotic, controlled drug or targeted substances which include changing the dose, formulation or regimen, and making a therapeutic substitution.
-
What is an “original” prescription?
An “original” prescription is an authorization from a practitioner to dispense a specified drug for use by a designated individual. Pharmacists may adapt an original prescription, including the first and subsequent refills of that prescription, in accordance with PPP-58. The adaptation does not need to be the beginning of a new drug therapy.
For the purposes of PPP-58, an original prescription may include a transferred prescription.
-
Can a community pharmacist accept a faxed prescription for a drug in the Controlled Prescription Program (CPP) that is not written on a CPP duplicate prescription form?
The CPP aims to reduce inappropriate prescribing of selected controlled drugs and to prevent forgeries. Prescriptions for the controlled drugs specified in the program must be written on the duplicate prescription pad specially developed for this purpose.
Verbal and faxed prescriptions for Schedule 1A drugs may not be accepted by a pharmacist in a community pharmacy; however, temporary amendments to the Pharmacy Operations and Drug Scheduling Act Bylaws and Community Pharmacy Standards of Practice are currently in place that allow the following:
Verbal Prescriptions:
- A registrant may only accept a verbal prescription for a drug listed in the CPP if doing so is permitted under a section 56 exemption to the Controlled Drugs and Substances Act. The pharmacy must receive either the original or a faxed copy of the CPP prescription form from the practitioner as soon as reasonably possible.
Faxed Prescriptions:
- A registrant may only accept a CPP prescription received by fax, during a public health emergency declared by the Provincial Health Officer. This includes the overdose crisis. Faxed prescriptions must still be written on a CPP form.
In both cases, the faxed copy of the CPP prescription received by the pharmacy must be written on a CPP duplicate prescription form, thus upholding the purpose of the CPP.
CPP duplicate prescription forms must still be used when using Electronic Medical Records (EMRs). As with all prescriptions, prescribers must ensure that all fields on the Controlled Prescription Program forms are completed correctly including those generated from an EMR. If the EMR is not capable of printing onto a CPP form, a copy of the completed CPP prescription form must be faxed as well.
-
When a pharmacist receives a verbal prescription for a drug in the Controlled Prescription Program (CPP), must the pharmacist wait to receive a faxed or hard copy of the CPP duplicate prescription form before dispensing the drug?
A pharmacist may dispense the CPP drug after receiving a verbal prescription. The pharmacy must receive the original prescription form, or a copy of the completed form transmitted by facsimile, from the practitioner as soon as reasonably possible after dispensing the drug.
-
Where can I access the College’s mandatory regulatory education module for PPMAC?
The College’s Pharmacist Prescribing for Minor Ailments and Contraception (PPMAC): Regulatory Education Module is available on UBC’s Canvas Catalogue Learning Management System.
-
Do I need to repeat taking the module annually?
The College only requires the module to be completed once to fulfill the education requirements. There is no requirement to repeat the module at this time.
-
Where do I declare that I have completed the module?
Declarations of module completion must be recorded in the registrant’s eServices account. Declarations can be submitted by selecting “My Profile” > “My Declarations” > “PPMAC”.
-
If I am a pharmacist who received authorization to prescribe in another province, do I still need to complete the College of Pharmacists of BC’s regulatory education module?
Yes. Prior to making a diagnosis and prescribing for minor ailments or contraception in BC, all pharmacists registered in BC who choose to provide services under PPMAC must complete the College’s regulatory education module and self-declare completion of this training through their eServices account.
The regulatory education module includes content specific to prescribing for minor ailments and contraception in BC.
-
Will completion of the module count towards my required accredited learning activities?
The College’s PPMAC regulatory education module is not an accredited learning program and therefore, cannot be used as an accredited learning activity for professional development. However, registrants may use the regulatory education module as a non-accredited learning activity.
-
Do I have to complete the module all in one sitting or can I complete part of it and then pick up later where I left off?
The regulatory module does not need to be completed in one sitting. Registrants may revisit the module as many times as required to pick up where they left off, until completed. Self-declaration through eServices must not be submitted until the module has been completed
-
Can a pharmacist’s prescription be transferred?
Yes. A pharmacist can transfer a prescription issued by a pharmacist, if the transfer is done in accordance with the Community Standards of Practice bylaws on prescription transfers.
-
Can a pharmacist prescribe Schedule II drugs for minor ailments?
No. The Regulation amendments do not give pharmacists authority to prescribe Schedule II drugs; however, Schedule II drugs can continue to be sold without a prescription, if the pharmacist determines it is appropriate for the patient.
-
Can a pharmacist adapt another pharmacist’s prescription?
Yes. A pharmacist can adapt another pharmacist’s prescription if the pharmacist determines that the adaptation meets the criteria in Professional Practice Policy – 58.
-
If I decide to advise a patient to seek treatment from another health professional rather than prescribe for the patient myself, do I still need to document and if so, what do I need to document?
According to Standard 14 of the HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions:
“A pharmacist who prescribes a drug for a patient must document…”
As stated, the documentation requirements only apply when a pharmacist prescribes a drug. However, the Ministry of Health may have its own PharmaCare policies regarding documentation when a patient assessment does not lead to a prescription being issued. Review of the Ministry of Health’s Pharmacare Policy Guide is recommended.
-
Can I diagnose and prescribe through phone or virtual consultation, or do I need to see the patient in person?
The HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions do not limit pharmacists to making diagnoses or prescribing for minor ailments or contraception in person.
A pharmacist may make a diagnosis and prescribe for a patient over the phone or through a virtual platform if the pharmacist is able to perform a patient assessment that is appropriate for the condition being treated and conducted in a manner that the patient confirms is suitably private for them. The pharmacist is responsible for ensuring that the patient’s identification is appropriately verified before providing any pharmacy service that requires accessing, collecting, using, or disclosing personal health information.
As always, when making a diagnosis or prescribing for a patient over the phone or through a virtual platform, pharmacists must continue to act in accordance with the:
- HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions;
- Conflict of Interest Standards;
- Code of Ethics; and
- Other relevant legislation, bylaws, and policies.
Note: The Ministry of Health may maintain its own requirements regarding the provision of PPMAC services to PharmaCare eligible patients. Review of the Ministry of Health’s Pharmacare Policy Guide is recommended.
-
Can pharmacists assess patients and prescribe in different practice settings other than licensed pharmacies?
The HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions do not prevent pharmacists from making a diagnosis or prescribing for minor ailments and contraception in settings outside of licensed pharmacies. However, when prescribing for patients in settings other than licensed pharmacies, pharmacists must continue to act in accordance with those standards and other relevant legislation, bylaws, and policies referred to in the Application section of the standards. Regardless of practice setting, pharmacists must confirm with the patient that the setting is suitably private for the patient.
In its recommendations to the College Board, the Prescribing and Drug Administration Committee (PDAC) of the College identified virtual care as an area that may require further regulation to ensure consistency in patient care. The standards, limits and conditions for virtual PPMAC services may be subject to change in the future.
-
Must PPMAC services be provided in a private consultation room?
According to Standard 11 of the College’s HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions: “When making a diagnosis or prescribing a drug, the pharmacist must take the appropriate steps to ensure the assessment is conducted in a manner that the patient confirms as suitably private.”
PPMAC services may be provided to patients in various practice settings and environments including community pharmacies, hospitals, or residential care facilities. It is the pharmacist’s responsibility to ensure that the patient’s privacy needs are addressed in any of these settings. As part of the process, it is important for the pharmacist to confirm with the patient that the space where the consultation will take place is suitably private for them before proceeding with the provision of any service, particularly if a private consultation room is not available.
-
Will pharmacists who are pharmacy owners be able to prescribe for “minor ailments” or contraception?
Yes. As of June 1, 2023, section 3 of the Pharmacy Operations General Regulation specifies that a pharmacist who is authorized to prescribe a drug may be a direct or indirect owner of a pharmacy. When prescribing, pharmacy owners must continue to act in accordance with the:
- HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions;
- Conflict of Interest Standards;
- Code of Ethics; and
- Other relevant legislation, bylaws, and policies.
-
Can a student pharmacist complete the assessment, make the diagnosis, prescribe a drug, and document if the pharmacist reviews and signs off on the prescription?
According to Standard 16 of the HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions:
“Only a full pharmacist may perform the restricted activities of making a diagnosis or prescribing a Schedule I drug and may only do so for the purposes set out in the Pharmacists Regulation”.
A pharmacy student who is a registrant of the College of Pharmacists of BC may provide pharmacy services under the supervision of a full pharmacist. As such, a pharmacy student registrant may participate in aspects of PPMAC; however, this must always be done under the supervision of a full pharmacist who has completed the required training and has self-declared the completion of their training through eServices. The supervising full pharmacist always has sole responsibility for the diagnosis and prescribing decisions.
Although pharmacy student registrants are not required to complete the regulatory education module prior to participating in aspects of PPMAC services, the module is available to pharmacy students, and they are encouraged to review the module to ensure a thorough understanding of the legislative framework that governs PPMAC in BC.
-
Is access to CareConnect required to prescribe under PPMAC?
Access to CareConnect is not a mandatory requirement for providing PPMAC services.
Standard 9 of the College’s Making a Diagnosis and Prescribing Standards, Limits and Conditions states:
“Prior to prescribing a drug, a pharmacist must obtain relevant drug therapy information, which may include a review of:
- the patient or resident record1;
- the patient PharmaNet record; or
- information provided by the patient or patient’s representative.”
Standard 10 of the College’s Making a Diagnosis and Prescribing Standards, Limits and Conditions states:
“A pharmacist must review or conduct a patient assessment to support their diagnosis and/or prescribing decisions. The assessment must include the following as feasible and applicable, but is not limited to these factors:
- demographic information;
- medical conditions;
- medication history;
- signs and symptoms;
- allergies and intolerances;
- risk factors;
- pregnancy and lactation status;
- physical assessment;
- laboratory or other diagnostic tests, if available;
- patient needs, values, and preferences; and
- any other information deemed necessary.”
The pharmacist is responsible for ensuring they have obtained the relevant drug therapy information and that they conduct a patient assessment to support their diagnosis and/or prescribing decisions. The pharmacist must use their professional judgement to determine how and where they access relevant information that is sufficient for informing and supporting their prescribing decision. This includes considering whether the patient’s CareConnect records need to be included in the review.
-
Are pharmacists limited to prescribing specific drugs for each minor ailment or contraception?
Under section 4(1)(a.2) of the Pharmacists Regulation, pharmacists can:
“for the purpose of treating a disease, disorder or condition diagnosed under paragraph (a.1), prescribe a drug that is
- specified in Schedule I of the Drug Schedules Regulation, and
- within a drug category shown opposite the disease, disorder or condition in Column 2 of Schedule A"
While there is no list of specific drugs that a pharmacist is limited to prescribing from for the purpose of treating a minor ailment, pharmacists must refer to Schedule A of the Pharmacists Regulation and are responsible for ensuring that the prescribed drug is included within the drug category corresponding to that condition and is appropriate for the patient and condition being treated.
-
Do I need additional liability insurance to make a diagnosis and prescribe for minor ailments and contraception?
The College does not require pharmacists to obtain additional liability insurance if they choose to diagnose or prescribe for minor ailments or contraception. Questions regarding liability coverage for the provision of PPMAC services should be directed to your insurance provider.<
-
Am I required to follow the medSask prescribing guidelines? Is there any particular guideline that I must follow?
MedSask is available to registrants as a clinical reference tool only. It is important to note that the medSask materials may not reflect the standards, limits and conditions set out by the College of Pharmacists of BC, or the requirements set out in the Pharmacists Regulation or the Ministry of Health’s Pharmacare Policy Guide. The Pharmacists Regulation sets out which conditions pharmacists may prescribe for, and the Schedule I drug categories pharmacists may prescribe for those conditions, which may be different than the medSask guidelines. Pharmacists are responsible for understanding and following the regulatory requirements for prescribing in BC.
-
Will all pharmacists provide PPMAC services?
Having the legislated authority to prescribe for minor ailments does not mean all pharmacists will offer or provide this service. Patients are encouraged to speak to their pharmacist to find out what healthcare services they offer and whether they are right for their needs.
The decision to incorporate prescribing for minor ailments into pharmacist practice, and to what extent, is based on the pharmacist’s clinical knowledge, skills, and judgment as well as the suitability of the practice environment, current circumstances, capacity, and comfort level. The decision to prescribe is at the discretion of the individual pharmacist, subject to the Code of Ethics.
Portions of the Code of Ethics that are especially relevant include:
- Section 1(b): “Registrants practice only within the scope of their education, training and competence”; and
- Section 1(g)(ii): “Registrants must provide pharmacy services requested by patients and may only refuse to provide these services for the following reasons: … the registrant does not possess the knowledge, skills and abilities to provide the service or product …”.
A pharmacist must complete the regulatory education requirement and self-declare completion in eServices prior to making a diagnosis or prescribing for a patient. A pharmacist who does not meet those requirements is not authorized to provide PPMAC services as they would not be practicing within the scope of their education, training and competence.
Additionally, a pharmacist who meets those requirements and decides to prescribe for minor ailments and contraception is not obligated to prescribe in every case. As with other health professionals, pharmacists will use their professional judgement to determine if they have the competency and confidence to prescribe in the best interest of the patient in each case.
-
What is considered a “minor ailment”?
Under section 4(1)(a.1) of the Pharmacists Regulation, pharmacists can:
“make a diagnosis identifying, as the cause of the signs or symptoms of an individual, a disease, disorder or condition that is shown in Column 1 of Schedule A, if all of the following conditions are met:
(i) the disease, disorder or condition, in the form indicated by the individual's signs and symptoms,
(A) presents a low risk of masking an underlying disease, disorder or condition, and
(B) can be readily diagnosed without the need for laboratory or imaging tests;
(ii) the individual's signs or symptoms can be reasonably expected to resolve with only short-term or episodic treatment”.
Pharmacists are responsible for determining if the condition being treated meets the criteria above, based on their professional judgement. Pharmacists may only prescribe for the diseases, disorders or conditions listed in Schedule A of the Pharmacists Regulation, if the criteria above are met.
-
Do I have to complete the regulatory education module before I can prescribe for minor ailments and contraception?
Yes. Prior to making a diagnosis or prescribing for minor ailments or contraception, pharmacists must complete the College’s regulatory education module and self-declare completion of this training through their eServices account. The module and self-declaration must be completed prior to providing services under PPMAC.
The College’s PPMAC Regulatory Education Module is the only mandatory training module that must be completed prior to providing PPMAC services. This requirement is found in Professional Practice Policy -70 Making a Diagnosis and Prescribing – Regulatory Education Module.
-
Can a pharmacist make a diagnosis and prescribe using an assessment conducted by another health professional, such as a nurse or another pharmacist?
According to Standard 10 of the HPA Bylaws Schedule F Part 8 – Making a Diagnosis and Prescribing Standards, Limits and Conditions:
“A pharmacist must review or conduct a patient assessment to support their diagnosis and/or prescribing decisions. The assessment must include the following as feasible and applicable, but is not limited to these factors…”
A pharmacist can review a patient assessment conducted by another health professional and use that assessment to support the pharmacist’s own diagnosis and prescribing decisions. A pharmacist is expected to use their professional judgment to determine if using another health professional’s assessment, would be appropriate and to ensure they have all the necessary information to make a diagnosis or prescribing decision that is safe and in the best interest of the patient.
In this situation, the pharmacist who diagnoses and prescribes for the patient is still required to follow the Standards, Limits and Conditions, including obtaining the patient’s or patient representative’s informed consent, having appropriate understanding of the patient need, providing the patient with drug information including patient-specific information, and establishing and documenting a follow-up and monitoring plan.
A pharmacist who makes a diagnosis or prescribes a drug is solely responsible for their treatment decision.
-
What is the difference between accredited and non-accredited hours?
Accredited learning activities have been reviewed using stringent criteria to ensure they are of high quality, unbiased, and clearly identify learning objectives for participants. Accredited programs indicate the number of accredited hours assigned, and identify the accrediting body (such as CCCEP, UBC CPPD, ACPE, MAINPRO, etc.). Supporting documentation that states the registrant’s name, the accrediting body, the number of accredited hours assigned, the date of completion, date accreditation is valid until, etc. is received upon successful completion.
Non-accredited hours are accumulated through informal learning. If you are doing self-study or on the job training, this will be classified as non-accredited hours. For example, if you identify a learning need in the area of compounding, and you choose to read a publication on compounding and incorporate this learning into your practice, you can document the actual time spent on the learning activity using increments of 0.25 hours (15 minutes).
-
Is it acceptable for prescribers to issue blanket authorizations for carries “on holidays” or “when the pharmacy is closed” for OAT prescriptions?
Prescription authorizations must always be patient-specific, taking into consideration the needs of the individual patient. As such, blanket authorizations applied to more than one patient are not acceptable. The indicated directions on any prescription must always be expressed in a manner that makes the intent of the prescriber clear. Instructions that authorize carries “on holidays” or “when the pharmacy is closed” are ambiguous as they lack the specificity required to determine the number of days the patient is allowed to carry. For instance, if a pharmacy is closed for three days per week, the patient would receive three carries. Conversely, if a pharmacy is closed for one day per week, the patient would only receive one carry. A prescriber must ensure that they are providing directions that clearly indicate how many days the patient is authorized to carry.
-
Can prescriptions be destroyed after scanning and storing electronically?
MOST prescriptions may be destroyed after scanning and storing, as long as all notes made on the prescription are captured in the colour scan. As per Pharmacy Operations and Drug Scheduling Act Bylaws s.23.3(1): “A pharmacy may maintain electronic records containing personal health information if the pharmacy has the equipment, software and systems necessary for the input, storage, use, protection and retrieval of records that are required to be kept under bylaws of the college or other legislation that regulates the practice of pharmacy.”
However, if the pharmacy has received an original or a faxed Controlled Prescription Program (CPP) form, then it must be retained, regardless of whether the form has been stored electronically.
It is also recommended that pharmacies confirm with other parties such as Pharmacare and third-party insurers to ensure retention requirements for audit purposes are met.
-
Do all pharmacies dispense Mifegymiso?
Any pharmacy where pharmacy professionals have the appropriate knowledge, skills and abilities, may dispense Mifegymiso®.
If a pharmacist declines to dispense Mifegymiso® on the basis of a conscientious objection, they are required to adhere to the Colleges’ Code of Ethics, Standard 1 (g)(iii), cooperating in effective transfers of care initiated by the patient (without needing to make a referral). Pharmacies must also have a process in place to ensure that, in the case where a pharmacy professional conscientiously objects to providing a service, the patient can be directed to an alternate provider for the service in a timely manner.
Learn more about the options for providing Mifegymiso® to patients in BC at bcpharmacists.org/mifegymiso.
-
We were working on a prescription for a narcotic liquid and the bottle tipped over. The contents spilled onto the counter and floor - what should I do?
To determine whether a loss should be reported and how to document, please see Health Canada’s Guidance on reporting loss or theft of controlled substances and precursors.
-
Can a pharmacist accept a prescription for a Schedule 1A drug (Controlled Prescription Program) written by an out-of-province physician?
In certain exceptional circumstances, a pharmacist can dispense a prescription for a Controlled Prescription Program (CPP) drug from an out-of-province physician or Canadian Armed Forces (CAF) physician practitioner that's not on the Controlled Prescription Program form. In these situations, as with any exceptional cases, the pharmacist must use their professional judgment in their decision to dispense. The pharmacist can base their decision on the medical condition of their patient and surrounding circumstances.
However, it is the pharmacist’s responsibility to ensure that the prescription is legitimate, and that the practitioner is licensed to practise medicine, podiatry or veterinary medicine in Canada. It may be reasonable for some patients, for example those who live close to the B.C./Alberta border, to have a physician in Alberta, and their pharmacy in B.C. In those cases, it may be appropriate to continue to dispense a controlled drug prescription from outside of B.C.
In most other circumstances, however, if a particular patient makes a habit of asking for drugs without a CPP form, the pharmacist should refer the patient to a practitioner licensed to practise in B.C. or a CAF physician with CPP forms. Pharmacists should not continue to dispense the prescriptions.
-
A deceased patient's wife recently brought the patient's unused narcotic medications to my pharmacy. Do I have to obtain authorization from Health Canada before I can destroy these narcotics?
Although the pharmacist accepts legal responsibility for the drug and its destruction, Health Canada no longer requires pharmacies to request and receive pre-authorization for local destruction of unserviceable narcotics and controlled drugs. This means that pharmacists may proceed with destruction without notifying and receiving acknowledgment from Health Canada in advance. All other requirements, including documentation, remain in place.
-
Why does it take so long to get my prescription filled?
There is a lot more to preparing your prescription than counting pills, typing a label and sticking it on a container. Your pharmacist checks the medication, dose and instructions to make sure they are right for you. They review your medical information and PharmaNet profile to check for possible problems. This may include allergies or interactions with other medications you are taking. Your pharmacist enters the details of your current prescription onto your PharmaNet profile. The prescription is then filled and undergoes a final check before being dispensed. Counselling must also be provided to give you information such as how and when to take your medication, what potential side effects you may need to watch for and how to store your medication.
-
How can I find out if the cost of my drugs is covered?
BC’s Pharmacare Program is responsible for the public coverage of medications for BC residents. You can learn more on their website: https://www2.gov.bc.ca/gov/content/health/health-drug-coverage/pharmacare-for-bc-residents
-
Do the patient and pharmacist need to sign to confirm the release of Opioid Agonist Treatment (i.e. methadone, morphine or buprenorphine for maintenance)?
Yes, prior to releasing the first OAT dose of a prescription, the pharmacist and the patient must sign the Controlled Prescription Program form in the space at the bottom of the form to confirm the patient has received the first dose of the prescription. The patient and pharmacist must also sign the patient/prescription-specific log to acknowledge the receipt of each witnessed ingestion dose, each partial dose and each take- home dose.
Neither the pharmacist nor the patient is permitted to pre-sign for future doses. The pharmacist must store the signed prescription and the patient/prescription-specific log together.
-
Do I have to dispense carries for methadone 10 mg/ml in individual bottles?
Each dose of methadone for opioid agonist treatment must be measured and dispensed in individually labelled, appropriately sized, child resistant packaging with an explicit warning label indicating that the amount of drug in the container could cause serious harm or toxicity if taken by someone other than the patient. It is not acceptable to dispense multiple carries in one container and have the patient measure individual doses at home.
-
Does Professional Practice Policy 66 apply to methadone, slow-release oral morphine or buprenorphine/naloxone, when used for pain?
No. PPP-66 sets the standards for dispensing methadone, SROM and buprenorphine/naloxone for opioid agonist treatment only. Prescriptions written for pain management must follow other non-OAT standards and policies.
-
Can a pharmacist accept a faxed or verbal OAT prescription?
Prescriptions for OAT may only be received by facsimile in accordance with section 7(3) of the Health Professions Act Bylaws Schedule F, Part 1 – Community Pharmacy Standards of Practice. A Controlled Prescription Program (CPP) form can only be accepted by facsimile during a public health emergency declared by the Provincial Health Officer. This includes the ongoing Overdose Crisis declared under the Public Health Act.
In addition, faxed methadone prescriptions can also be accepted under extenuating circumstances where the prescriber has determined, following consultation with the pharmacist, that the urgency of the situation warrants it.
Prescriptions may only be accepted verbally when permitted under a section 56 exemption to the Controlled Drugs and Substances Act in accordance with section 19(6.1) of the bylaws to the Pharmacy Operations and Drug Scheduling Act. The pharmacy must receive either the original or a faxed copy of the CPP prescription form from the prescriber as soon as reasonably possible.
-
I recently completed a Practice Review. Can I use that towards my Continuing Education (CE) requirements?
You can include any educational activities undertaken to prepare for the Practice Reviews, or as a result of the Practice Review towards your CE requirements and record them accordingly on the PDAP Portal.
For example: if you read the comprehensive outlines of focus areas for Pharmacy Professionals Reviews on the PRP Support Tools in order to get ready for the Practice Review, you would record that as non-accredited learning and document the actual time spent on the activity.
-
When are my Continuing Education (CE) submissions due?
Your CE Submissions along with all your other registration renewal requirements are due just before midnight on your registration renewal date. You renew registration for the following year by submitting your CE learning activities undertaken within the most recent 12 months of your registration renewal date.
For example, if your registration renewal date is August 31, 2020, to be able to renew registration for period September 1, 2020-August 31, 2021, you must submit through the PDAP Portal, CE activities undertaken during September 1, 2019-August 31, 2020, along with all other registration renewal requirements, at the latest by 11:59pm on August 31, 2020.
-
Do I have to have a specific amount of accredited vs non-accredited hours?
A minimum of 5 hours must be accredited learning and supporting documentation needs to be provided as part of the Learning Record (s) it pertains to. Supporting documentation that states the registrant’s name, the accrediting body, the number of accredited hours assigned, the date of completion, date accreditation is valid until, etc. is received upon successful completion. Document the hours the activity is accredited for under the “Accredited Hours” field in the PDAP Portal. Any additional time spent beyond what the activity is accredited for, can be recorded as “Non-Accredited Hours” using increments of 0.25 hours (15 minutes). Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
What is my current PDAP cycle?
The current PDAP cycle year is displayed on the PDAP Portal based on when your cycle started.
For example, if your registration renewal date is August 31, 2020, you must submit through the PDAP Portal, Continuing Education (CE) activities undertaken during September 1, 2019-August 31, 2020. Your current PDAP Cycle would be 2019.
-
What type of electronic files are accepted as supporting documentation?
The PDAP portal accepts common text and image file types such as .pdf, .txt, .doc, .docx, .jpeg, .jpg, .gif, .png. Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
-
How long should I retain my original supporting documentation?
Please retain all original supporting documentation for at least 2 years from your registration renewal deadline.
For example, if your registration renewal date is August 31, 2020, you must submit through the PDAP Portal, Continuing Education (CE) activities undertaken during September 1, 2019-August 31, 2020. You would keep the original supporting documentation at least until August 31, 2022
-
How will CE requirements be affected during the transition to a single renewal date?
At the first single renewal date (registration renewal deadline of March 31, 2025), submission of CE requirements will not be required to proceed with renewal.
A new cycle for completing CE will resume on April 1, 2025, and submission of CE will be required to renew registration on March 31, 2026.
Although CE will not need to be submitted at the registration renewal deadline of March 31, 2025, registrants are reminded of their ongoing responsibility under the Code of Ethics Standard 10(a) to “keep up to date with new pharmacy knowledge and practices by participating in continuous lifelong learning.” To support this, the PDAP portal will continue to be available for registrants to document and track their learning during the transition to the single renewal date. Any CE completed prior to April 1, 2025 cannot be carried over for your March 31, 2026 renewal.
-
How will the pro-rated fees be calculated for partial year registrations during the transition year?
The pro-rated fees are calculated based on the number of months from your current renewal date until the new single renewal date for all registrants in March 2025. A detailed breakdown of this calculation can be found in the table above.
-
Why is the College moving to a single renewal date for all registrants?
The College of Pharmacists of British Columbia is transitioning to a single renewal date to enhance operational efficiency and to support the College's administrative processes. This change supports the College in its mandate of protecting public health.
-
What is my pro-rated fee for the 2024-25 billing period?
The College is transitioning to a single renewal date for all registrants, which will be in place by March 31, 2025. During the transition in 2024, if your renewal date is after March 31, your fees will be prorated until March 2025.
Please refer to the pro-rated fee chart below for detailed information on the transition period fees.
-
How will the transition to a single renewal date affect my registration status during the transition year?
During the transition year, your registration status will remain as active, identical to any standard renewal process. So long as the pro-rated fees are paid, your CE requirements have been met, and there are no disciplinary actions affecting your status, there will be no difference from any other renewal year.
-
Will there be any changes to the continuing education requirements for 2024?
Currently, there are no changes to the CE requirements for 2024. Submission of CE continues to be mandatory for all pharmacy professionals to renew their registration on or before February 28, 2025.
-
Will there be changes to the requirements or process for renewing registration in the future?
There are no changes to the requirements or process for renewing registration.
-
What will be the Continuing Education requirements starting April 1, 2025?
At this time, there are no changes to CE requirements after the transition to a single renewal date. Registrants will be required to submit their CE once the single renewal date is implemented.
-
Can pharmacists administer drugs or perform pharmacist/patient consultations from a remote location?
Pharmacy professionals may administer medications or provide consultations from any location where security, privacy and confidentiality can be maintained. They must make sure that proper conditions and equipment needs are met when providing these services (e.g. anaphylaxis kits). Please note that the storage of drugs and personal health information outside licensed pharmacy premises is restricted under the PODSA bylaws.
-
Can patients send in photos of their prescriptions to the pharmacy for dispensing?
Only fax transmission of prescriptions directly from the practitioner is allowed. Otherwise, the pharmacy must have an original prescription or have received a verbal prescription from a practitioner before dispensing prescription medications.
Useful links:
-
What should the pharmacy do if they receive a request for information from law enforcement? (e.g. video surveillance footage)
Information can be disclosed when complying with a court-ordered subpoena, warrant or order, or otherwise compelled by a person or body with appropriate jurisdiction. Also, you may disclose the information if you believe doing so will reduce a risk of significant harm to the health and safety of any person. This does not constitute legal advice, and we recommend you seek your own legal counsel. Please refer to the Health Professions Act Bylaws, section 72, for more information.
Useful links:
-
A family member of a deceased patient is asking for records related to prescriptions. Are pharmacy professionals allowed to release this information?
Pharmacy professionals must release personal health information if requested to do so by a person who is legally authorized, in writing, such as an executor of the estate.
Useful links:
-
An unexplained discrepancy was discovered with the pharmacy’s narcotic inventory. What should be done?
Unexplained losses of controlled drugs, including narcotic medications, must be reported to Health Canada within 10 days of discovery and a copy of the report sent to Health Canada must be forwarded to the College.
Useful links:
- Professional Practice Policy 74
- Health Canada guidance on reporting loss or theft of controlled substances and precursors
-
Can practitioners use another practitioner’s Controlled Prescription Program (CPP) form?
No, practitioners must use the Controlled Prescription Program form they were issued. If a practitioner has not defined a place of practice, the form will be missing the practice address, but the name and the registration number will be printed on the form.
-
What are the bylaws or policies that regulate online/internet pharmacy operations?
There are currently no additional bylaws or policies that regulate online pharmacy operations. Any pharmacies located and operating in BC must comply with all existing legislation.
-
A patient is requesting the remaining 3 months of a refill on a prescription that expires next week. Are pharmacists allowed to dispense the full 3 months?
The Community Pharmacy Standards of Practice state that a registrant must not dispense prescriptions more than two years from the prescribing date, but it does not limit the duration of therapy that may be dispensed. However, pharmacists must use their professional judgement to assess the appropriateness prior to dispensing any prescription.
Useful links:
-
Is a cover letter required when receiving faxed prescriptions?
The fax cover letter is not a requirement of pharmacy record-keeping, however it may contain information required by bylaws that is not on the prescription. For a faxed prescription to be valid, it must have the practitioner’s phone number, fax number, time/date of transmission, pharmacy name and pharmacy fax number.
Useful links:
-
Can all refills be combined when filling a prescription? For example, if the prescription is written 90 tablets + 3 refills, can all 360 tablets be dispensed at once?
Pharmacists may reduce the dispensing quantity in some cases, but they are expected to dispense the prescription as written by the practitioner. Otherwise, pharmacists must consult with the prescriber before adjusting quantities to be dispensed.
Useful links:
-
What are the restrictions to providing an emergency supply?
There are no restrictions based on drug schedule or indication for an emergency supply. However, pharmacists must only provide it if they have the appropriate knowledge, sufficient information, and informed consent from the patient.
Useful links:
-
Can a prescription written by a practitioner who is no longer active on Pharmanet be adapted?
One of the requirements for an adaptation involves notifying the original prescriber. If the original prescriber cannot be notified, an adaptation would not be appropriate.
Useful links:
-
Is there a maximum duration or number of OAT doses permitted for carries?
There are no maximum number of take-home doses for OAT specified in the policy guides, but pharmacists must assess the appropriateness of the quantity dispensed.
Useful links:
-
Can the pharmacist refuse to sell Tylenol #1 (acetaminophen, caffeine, codeine) to a patient?
Depending on the reason, pharmacists can refuse to sell Tylenol #1. Health Canada forbids the sale of low-dose codeine products if the pharmacist has reasonable grounds to believe that it is not being used for recognized medical or dental purposes. The pharmacist has an obligation to resolve any drug therapy problems when selling any Schedule II medications.
Useful links:
-
What is the procedure the pharmacy must follow when narcotic medications must be destroyed?
Please follow the instructions provided by Health Canada: https://www.canada.ca/en/health-canada/services/health-concerns/controlled-substances-precursor-chemicals/controlled-substances/compliance-monitoring/compliance-monitoring-controlled-substances/unserviceable-stock.html
Useful links:
-
Are pharmacists able to prescribe compounded prescription medications?
Neither the Pharmacists Regulation nor the College’s standards, limits and conditions for prescribing differentiate compounds versus non-compounds when it comes to prescribing. The compounded medication must be in the drug category specified in the regulations.